When your medication is keeping you awake-or making you groggy all day-you’re not alone. Millions of people take drugs for depression, high blood pressure, or insomnia itself, only to find their sleep getting worse, not better. It’s a cruel twist: the very pills meant to help you feel better end up sabotaging your rest. But there’s a powerful, science-backed way to fight back-not with more pills, but with sleep hygiene.
Why Your Medication Is Messing With Your Sleep
Not all medications affect sleep the same way. Some are too stimulating. Others blunt your body’s natural sleep signals. Even sleep aids can backfire. Antidepressants like fluoxetine (Prozac) are notorious for keeping people up at night. They boost serotonin, which can be energizing. But paroxetine (Paxil)? It often makes people sleepy. Same class, opposite effects. Beta blockers like metoprolol and atenolol, used for high blood pressure, reduce melatonin production by nearly 40%. That’s your body’s main sleep hormone. Less melatonin? Harder to fall asleep. And then there are the sleep medications themselves. Drugs like zolpidem (Ambien) and eszopiclone (Lunesta) may help you nod off-but they leave behind a foggy, clumsy morning. Studies show over two-thirds of users feel drowsy the next day. One in five report memory lapses or trouble focusing. Worse, some people have done things like sleep-driving or eating in their sleep without remembering it.What Sleep Hygiene Really Means (And Why It Works)
Sleep hygiene isn’t just about avoiding caffeine before bed. It’s a set of daily habits that reset your body’s internal clock and reduce the damage caused by medications. Backed by decades of research from the Mayo Clinic and the American Academy of Sleep Medicine, it’s the first-line defense-not a last resort. The goal? To strengthen your natural sleep drive so your body doesn’t have to rely on pills that come with dangerous side effects. In fact, long-term use of sleep meds like benzodiazepines and Z-drugs increases dementia risk by over 80%. Sleep hygiene helps you avoid that.Step-by-Step: Fixing Sleep When Medications Are the Problem
1. Lock in Your Wake-Up Time No matter what time you went to bed, wake up within 30 minutes of the same time every day-even on weekends. This is the single most powerful habit. Your circadian rhythm thrives on consistency. A 2022 JAMA study found that people who stuck to a fixed wake time improved their sleep efficiency by over 58% in just three weeks. If you’re on beta blockers or antidepressants that mess with your natural rhythm, this step is non-negotiable. 2. Control Light Like Your Life Depends On It Light is your body’s master clock. After 8 p.m., eliminate all blue light. Turn off TVs, phones, and tablets. Use dim red lights if you need to get up at night. In the morning, get 30 minutes of bright light-ideally 10,000 lux-within 15 minutes of waking. This counteracts the melatonin suppression caused by blood pressure meds. You don’t need sunlight. A light therapy box from a pharmacy works fine. 3. Time Your Exercise Right Working out is great for sleep-but not if you do it too late. Stimulating medications like SSRIs or stimulants for ADHD can make exercise at night feel like a caffeine shot. Do your workouts at least four hours before bed. Even a brisk walk after dinner helps, as long as it’s not close to bedtime. 4. Take Sleep Medications Only When You Can Sleep All Night If you’re on zolpidem, zaleplon, or eszopiclone, never take them unless you have 7-8 hours before you need to be awake. The FDA found that taking these drugs with less sleep time increases next-day impairment by 32%. If you’re waking up at 6 a.m., don’t take it after 10 p.m. If you’re sleeping in, plan ahead. Your brain doesn’t know you’re trying to “catch up.” It just knows you took a drug and didn’t give it time to clear. 5. Eat for Sleep, Not Just for Health Avoid aged cheeses, cured meats, and soy sauce if you’re on blood pressure meds. These are high in tyramine, which can spike your blood pressure and disrupt sleep. Instead, eat magnesium-rich foods: almonds, spinach, black beans, and pumpkin seeds. A 2020 study showed these cut insomnia severity by over 34%. Magnesium helps calm your nervous system-something many meds overstimulate. 6. Create a Medication Buffer Zone If you take a sleep aid, don’t just take it and crawl into bed. Wait at least two hours after taking it before you lie down. Why? Because sleep pressure builds slowly. If you go to bed right after taking a pill, your brain doesn’t have time to process it. This can make side effects worse. Use that buffer time to read a book in dim light or do light stretching.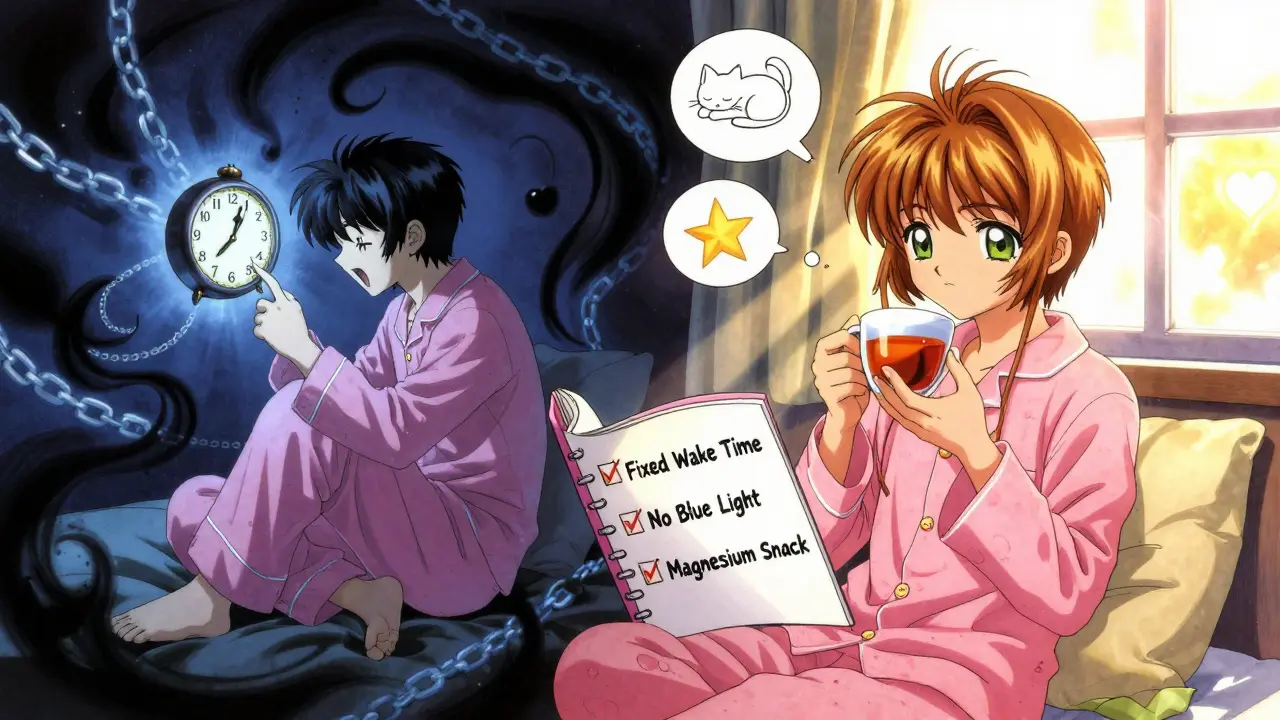
What Not to Do
Don’t try to “sleep in” to make up for bad nights. That ruins your wake-up routine and makes everything worse. Don’t rely on alcohol to help you sleep-it fragments sleep in the second half of the night. Don’t keep checking the clock. That anxiety alone can keep you awake. And don’t assume your doctor knows all the side effects. Many aren’t trained in sleep science. Bring this info to your next appointment.Real Results: People Who Got Their Sleep Back
On Reddit’s r/Insomnia forum, over 78% of users who followed a strict sleep hygiene routine reported less next-day grogginess from zolpidem within six weeks. One user, 62, stopped taking Ambien after years of morning confusion. She started waking at 6:30 a.m. sharp, used a light box, and ate almonds daily. Within 45 days, she stopped needing the pill. Her energy returned. Her memory cleared. The Sleepio CBT-I program tracked 2,315 people on sleep meds. Those who followed these hygiene steps saw a 71% drop in next-day impairment. Not because they took less medication-but because they stopped letting the medication win.
Why This Is the New Standard
The American College of Physicians now says CBT-I (a structured form of sleep hygiene) should be the first treatment for chronic insomnia-not pills. The FDA has issued black box warnings on sleep meds because of dangerous side effects. Twenty-eight U.S. states now require doctors to document sleep hygiene education before prescribing long-term sleep drugs. In Europe, benzodiazepines for insomnia are limited to four weeks. The tide has turned. And now, tech is catching up. Apple’s iOS 17 Health app now flags your medications and gives you a personalized sleep hygiene score. In trials, users who followed the app’s advice saw a 41% drop in medication-related sleep complaints.Start Small. Stick With It.
You don’t need to fix everything at once. Pick one thing: maybe it’s waking up at the same time every day. Do that for three weeks. Then add light exposure in the morning. Then cut blue light after 8 p.m. Each small change adds up. Medications are powerful. But your body’s natural rhythm is stronger. You don’t need more pills. You need better habits.Can sleep hygiene replace my sleep medication entirely?
For many people, yes-but not without medical supervision. Sleep hygiene doesn’t eliminate the need for medication in all cases, but it often reduces the dose needed or makes the medication safer to use. In some cases, people stop taking sleep meds altogether after 6-12 weeks of consistent hygiene practices. Always work with your doctor before making changes.
Why does waking up at the same time matter so much?
Your body’s internal clock runs on consistency. Even one late morning can throw off your melatonin rhythm for days. Medications like beta blockers or antidepressants already disrupt this rhythm. A fixed wake time is the anchor that pulls it back. Studies show this single habit improves sleep efficiency more than any other behavioral change.
I take blood pressure meds. Why should I avoid aged cheese?
Aged cheeses, cured meats, and soy sauce contain tyramine, a compound that can spike blood pressure. If you’re on beta blockers or ACE inhibitors, this can interfere with your medication’s effect and trigger nighttime awakenings. It’s not just about sleep-it’s about safety. Avoiding these foods reduces stress on your cardiovascular system while helping you sleep.
Is it safe to use light therapy if I have eye problems?
Most people with eye conditions like glaucoma or macular degeneration can safely use light therapy, but it’s best to check with your ophthalmologist first. Use a standard 10,000 lux box positioned at eye level, not staring directly into it. The light doesn’t need to be bright enough to hurt your eyes-it just needs to reach your retina to signal your brain it’s morning.
How long before I see results from sleep hygiene?
Most people notice improvements in 2-3 weeks. Deep changes-like reduced next-day grogginess or fewer nighttime awakenings-take 4-6 weeks. The key is consistency. Missing a day or two won’t ruin progress, but going back to old habits will. Think of it like physical therapy for your sleep.
What if my medication schedule changes?
If your medication timing shifts-say, you switch from morning to evening dosing-adjust your sleep hygiene routine around it. For example, if you start taking a stimulant in the afternoon, move your exercise earlier and be extra strict about light exposure after 7 p.m. Your body adapts, but you need to adapt with it.








11 Comments
Sonja Stoces
February 14, 2026 AT 04:50I tried all this "sleep hygiene" crap. Woke up at 6:30 a.m. like a robot, used a light box, ate almonds... and still took 3 hours to fall asleep. My Prozac is the real villain here. Not my circadian rhythm. Not my phone. My meds. Why is no one talking about just switching meds instead of making me into a sleep monk? 😒
Suzette Smith
February 15, 2026 AT 05:47I love how this post treats sleep hygiene like magic beans. But what if you work nights? Or have a kid who wakes up at 3 a.m.? Not everyone gets to pick their schedule. Just saying. 🌞
Reggie McIntyre
February 16, 2026 AT 05:08This is the most beautifully practical thing I’ve read all year. Like someone took the scattered pieces of my sleep-deprived brain and glued them back together with science. I started locking in my wake time-no exceptions-and within 10 days, I stopped needing Ambien. My brain feels like it’s been unplugged from a static storm. Also, light therapy? Game changer. I’m now weirdly obsessed with my 10,000 lux box. It’s my morning coffee. ☀️
Jack Havard
February 17, 2026 AT 09:39You’re telling me the FDA and Mayo Clinic are suddenly the gospel on sleep? Meanwhile, the same institutions pushed opioids for pain and antidepressants as first-line for everything. This is just another corporate-backed fad dressed up as wisdom. I’ll take my melatonin and my 3 a.m. TikTok scrolls, thanks.
Gloria Ricky
February 18, 2026 AT 21:26I just started step 1-waking up at the same time-and honestly? It’s weirdly hard. I thought I was a morning person until I tried to be one on purpose. But I’m trying. One day at a time. Also, the almond thing? I’m eating them like popcorn now. My snack game has upgraded. 🥜
Stacie Willhite
February 20, 2026 AT 17:47I’ve been on beta blockers for 8 years. Never knew they were killing my melatonin. This post made me cry. Not because it’s sad-because it’s the first time someone explained why I’ve felt like a zombie since 2016. Thank you. I’m getting a light box tomorrow.
Jason Pascoe
February 22, 2026 AT 08:09I live in Australia and we don’t have the same access to light therapy boxes. But I’ve been using my backyard sunrise instead-no filter, no screen, just me and the dawn. It’s not perfect, but it’s something. Also, the tyramine warning? Huge. I used to snack on parmesan before bed. No more. My sleep’s been quieter since.
christian jon
February 22, 2026 AT 16:49Let me just say this: If you’re following this advice and still sleeping poorly, you’re doing it wrong. PERIOD. You’re not trying hard enough. You need discipline. Not just "eating almonds." You need a 5 a.m. wake-up, a 10 p.m. lights-out, a 30-minute cold shower before bed, and a journal entry on why you deserve rest. If you’re not doing all of that, you’re just whining. And yes-I’ve read every study. I’ve seen the data. You’re not special. Your sleep isn’t broken. YOU are.
Pat Mun
February 23, 2026 AT 21:29I’ve been doing most of this for 6 weeks now. Woke up at 6:30, no phone after 8, magnesium before bed, and I swear-I didn’t even notice I’d stopped taking my zolpidem. It just… faded out. Like my body remembered how to sleep without being forced. I’m not saying it’s easy. But it’s worth it. And honestly? I feel like a new person. Not because of the science-because I finally stopped fighting myself. 🌿
Sophia Nelson
February 25, 2026 AT 04:57This whole post is a glorified wellness influencer fantasy. You think people on beta blockers just need to eat almonds? What about the ones with chronic pain? Or PTSD? Or shift work? This advice is for rich, white, able-bodied people who have 8 hours to waste on sleep optimization. Meanwhile, I’m taking 3 meds and working two jobs. Thanks for the lecture, though.
Skilken Awe
February 26, 2026 AT 11:33Sleep hygiene? More like sleep shaming. You’ve got a 2022 JAMA study? I’ve got a 2023 meta-analysis from the BMJ showing CBT-I has a 38% dropout rate because it’s unsustainable for anyone with a real life. And you’re telling me to wait two hours after taking zolpidem? That’s not sleep hygiene-that’s a fucking obstacle course. You’re pathologizing normal human biology. Stop selling this as a cure. It’s a Band-Aid on a hemorrhage.