When the temperature hits 24°C (75°F) or higher, your body is already under stress. For someone using drugs, that stress can turn deadly. Heatwaves don’t just make you sweaty and tired-they change how your body processes drugs, increasing the chance of overdose even if you’re using the same amount you always have. This isn’t theoretical. In New York City, emergency calls for overdoses jumped 22% during heat advisories between 2018 and 2022. In the Pacific Northwest’s 2021 heat dome, overdose deaths spiked sharply in places that rarely see extreme heat. The connection is real, and it’s deadly. But it’s also preventable.
Why Heat Makes Overdose More Likely
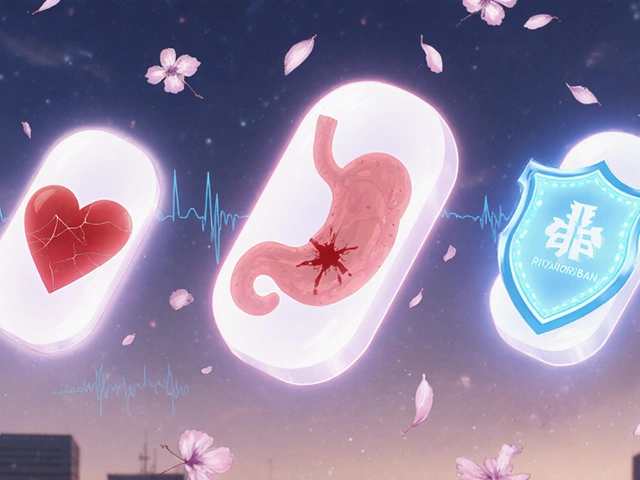
Your body works hard to stay cool. When it’s hot, your heart pumps faster-up to 25 beats per minute more at rest. If you’re using stimulants like cocaine or meth, your heart is already racing. Add heat, and you’re pushing your cardiovascular system past its limit. Studies show this combination can trigger heart attacks or strokes even in younger people with no prior history. Dehydration plays a big role too. When you lose just 2% of your body weight in fluids-something easy to do in hot weather-your blood gets thicker. That means the same dose of a drug becomes more concentrated. A 100mg dose of heroin or fentanyl might as well be 120mg. That’s not a guess. It’s measured in lab studies. And it’s why people who’ve used the same dose for years suddenly overdose on a hot day. Opioids are especially dangerous in heat. Your body normally compensates for their respiratory-depressing effects by breathing deeper. Heat weakens that response by 12-18%. You might not even realize you’re slowing your breathing until it’s too late. Meanwhile, many psychiatric medications-like antipsychotics and antidepressants-lose effectiveness in heat, making mental health symptoms worse. That can lead to using more drugs to cope, increasing overdose risk even further.Who’s Most at Risk
People experiencing homelessness are hit hardest. About 580,000 people in the U.S. live on the streets or in shelters. Nearly 40% of them have a substance use disorder. These individuals often can’t access air-conditioned spaces, clean water, or medical care. During a heatwave, they’re exposed to temperatures 3-5°C higher than surrounding areas because of urban heat islands-concrete, asphalt, and buildings trapping heat. People taking medications for mental health conditions are also at higher risk. About 70% of antipsychotics and 45% of antidepressants interact poorly with heat. Side effects like dizziness, confusion, and rapid heartbeat get worse. That makes it harder to recognize early signs of heat illness or overdose. Many don’t know their meds are making them more vulnerable. And it’s not just street drugs. Prescription opioids, benzodiazepines, and even alcohol can become more dangerous in heat. A person managing chronic pain with opioids might not realize their dose is now too high because their body can’t regulate temperature the way it used to.
What You Can Do: Practical Harm Reduction Steps
You don’t need to stop using drugs to stay safe. Harm reduction means reducing risk-not eliminating behavior. Here’s what works:- Reduce your dose by 25-30% when it’s above 24°C. This isn’t arbitrary. It’s based on how much your body’s ability to metabolize drugs changes in heat. Even if you’ve used the same amount for years, your body isn’t the same in a heatwave.
- Drink one cup of cool water every 20 minutes. Not soda. Not energy drinks. Plain water at 50-60°F. This helps your body flush toxins and keeps your blood from thickening. NYC’s Harm Reduction Coalition saw a 17% drop in heat-related overdose calls after pushing this simple rule.
- Avoid using alone. If you’re using, have someone nearby who knows how to use naloxone. If you’re alone, text a friend before you use and set a timer to check in. If they don’t hear from you, they call 911.
- Use in a cool space. If you can’t get indoors, find shade. Use a damp towel on your neck. Carry a small misting bottle with water. Cooling your skin lowers your core temperature, even slightly.
- Know your meds. If you take any prescription drugs for depression, anxiety, psychosis, or chronic pain, talk to your provider before summer hits. Ask: Does this interact with heat? Some need dose adjustments.
What Communities and Services Can Do
Individual actions save lives, but systems need to change too. Right now, only 12 of 50 U.S. states have heat emergency plans that include people who use drugs. That’s unacceptable. Effective models already exist:- Philadelphia’s Cooling Kits-distributed to over 2,500 people annually-include electrolyte packets, misting towels, water bottles, and overdose prevention cards. No ID needed. No judgment.
- Vancouver’s Cooling and Care Centers combine air-conditioned rest spaces with supervised consumption sites. During the 2021 heat dome, they cut heat-related overdose deaths by 34%.
- Maricopa County’s Check-in Programs trained volunteers to knock on doors of people living outdoors. They carried naloxone, water, and cooling supplies. In 2022, they made over 12,000 wellness checks and reversed 287 overdoses.
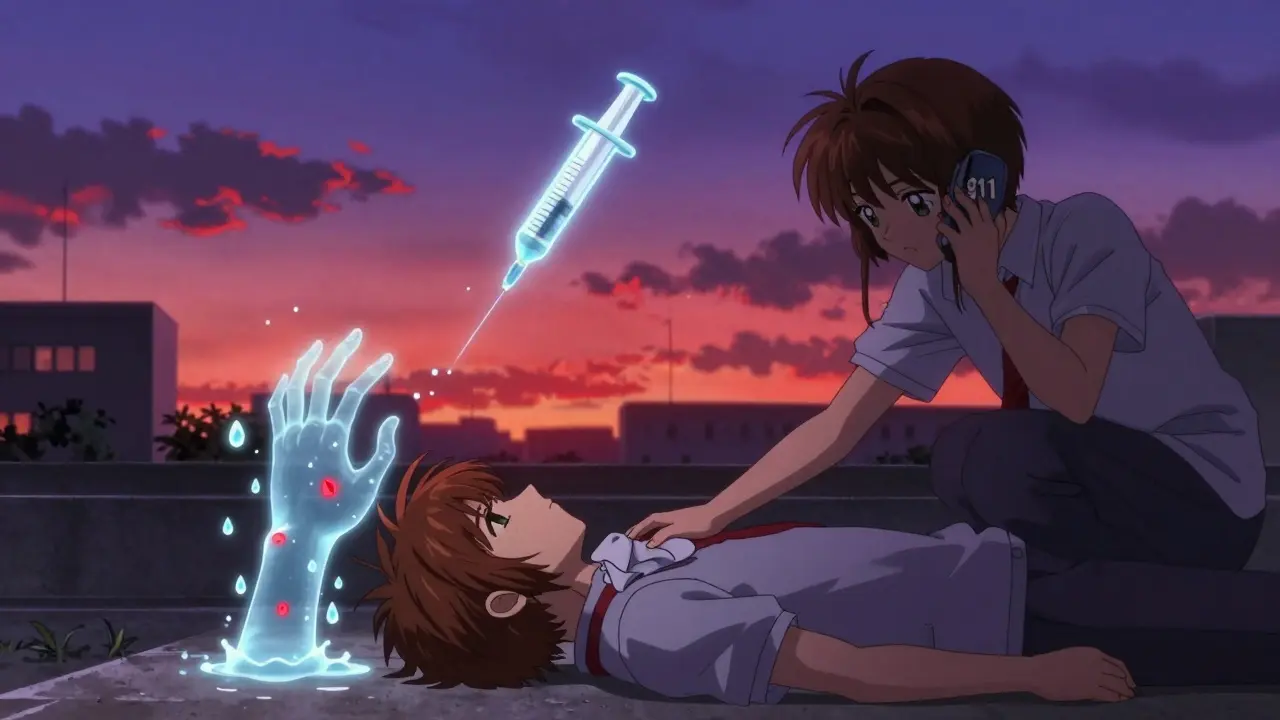
What to Do If Someone Overdoses in the Heat
If you see someone unresponsive, blue, or breathing shallowly:- Call 911 immediately. Say: “Person overdosing, possible heat exposure.” This helps responders prepare.
- Give naloxone if available. Even if you think it’s just heat illness, naloxone won’t hurt if opioids aren’t involved.
- Move them to shade or a cooler area. Remove excess clothing.
- Apply cool, wet cloths to their neck, armpits, and groin. Don’t ice them down-this can cause shock.
- Keep them on their side if they’re unconscious. This prevents choking.
- Stay with them until help arrives.
What’s Changing in 2025 and Beyond
By 2050, climate models predict 20-30 more days each year above the 24°C overdose risk threshold. That means more people will be at risk, more often. The Biden administration has allocated $50 million to fix this. By December 2025, every state health department must include overdose risk in their heat emergency plans. New research is also emerging. Scientists are finding that extreme heat changes gut bacteria by 15-20%, which could alter how drugs are broken down in the body. That might mean future harm reduction guidelines will need to include personalized advice based on diet, medication, and even microbiome health. The bottom line: heatwaves are no longer just a summer inconvenience. They’re a public health emergency that kills people who use drugs. And the solutions exist. We just need to scale them up.Can drinking water really prevent an overdose during a heatwave?
Yes, but not alone. Drinking water helps prevent dehydration, which concentrates drugs in your blood and raises overdose risk. One cup every 20 minutes can reduce that risk by up to 17%, according to real-world programs in New York City. But water isn’t a magic fix-it works best with other steps like reducing your dose, staying cool, and not using alone.
I’m on medication for depression. Should I be worried about heat?
Yes. About 70% of antipsychotics and 45% of antidepressants become less effective or cause worse side effects in heat, like dizziness, confusion, or rapid heartbeat. These symptoms can mask early signs of overdose or heat illness. Talk to your doctor before summer. Ask if your meds need adjustment during hot weather.
Why do overdoses spike more in cooler cities during heatwaves?
People in cooler places like the Pacific Northwest aren’t used to extreme heat. Their bodies haven’t adapted. So when temperatures hit 35°C, their systems shut down faster than someone in Arizona who’s lived with heat for years. That’s why overdose risk can be 3.7 times higher in cities with no history of heatwaves compared to 2.1 times in hotter regions.
Can I still use drugs safely during a heatwave?
There’s no completely safe way to use drugs, but you can reduce risk dramatically. Reduce your dose by 25-30%, drink water every 20 minutes, use in a cool place, and never use alone. These steps have been proven to cut heat-related overdoses. Harm reduction isn’t about quitting-it’s about staying alive.
Are shelters safe during heatwaves?
Many aren’t. Some shelters turn away people who are actively using drugs, even during heat emergencies. Others have no air conditioning. If you’re homeless and concerned about heat, look for cooling centers-these are often run by public health departments or harm reduction groups and don’t require sobriety. In Vancouver and Philadelphia, they’re open to everyone.
What’s in a cooling kit?
A typical cooling kit includes electrolyte packets (to replace lost salts), a misting spray bottle, a damp cooling towel, bottled water, and a card with overdose prevention info and naloxone instructions. Some include sunscreen or a small fan. These kits are distributed for free by harm reduction organizations and public health agencies. No ID or proof of need required.
Is naloxone still effective in heat?
Yes. Naloxone works the same way regardless of temperature. But it’s critical to act fast. Heat can cause organ failure faster than opioid overdose alone. If someone is unresponsive, give naloxone, call 911, and cool them down immediately. Don’t wait to see if it works-heat is a silent killer.
How do I find a cooling center near me?
Call your local public health department or search for “cooling centers” + your city name. Many are listed on city websites during heat advisories. Harm reduction organizations like the Harm Reduction Coalition or local needle exchanges often know where they are. Some are co-located with supervised consumption sites and offer water, rest, and overdose reversal tools-all without judgment.







14 Comments
Margaret Khaemba
January 21, 2026 AT 12:41This is honestly one of the most practical harm reduction guides I've seen in years. I work with unhoused folks in Philly and we hand out those cooling kits every summer. The water rule alone? Game changer. People don’t realize how fast dehydration turns a manageable high into a hospital trip. Just last week, a guy told me he’d been using the same dose for 4 years-then hit 90°F and nearly didn’t make it. He’s now carrying a water bottle everywhere. Small change, huge difference.
Also, the gut bacteria thing? Wild. I’ve been reading up on microbiome shifts in heat. Could explain why some folks suddenly react differently even with the same drug. We’re gonna need way more research on this.
Also-why isn’t this in every ER triage protocol? It should be standard.
Thanks for writing this.
Malik Ronquillo
January 23, 2026 AT 07:37Wow. So now we’re treating drug use like it’s a weather advisory? Next they’ll be giving out sunscreen and SPF ratings for fentanyl.
I mean, sure, drink water. But this whole thing feels like coddling. If you’re dumb enough to use drugs in a heatwave, maybe you shouldn’t be alive. Just sayin’.
Liberty C
January 23, 2026 AT 20:49Let’s be real: this isn’t harm reduction-it’s harm glorification dressed in public health jargon. You’re not ‘reducing risk,’ you’re enabling a behavioral pathology under the guise of compassion. The fact that we’re now quantifying how much water to drink while shooting up instead of addressing the root causes of addiction speaks volumes about our cultural decay. We’ve replaced moral accountability with hydration schedules.
And don’t get me started on ‘cooling kits’-next they’ll be handing out velvet pillows for your overdose. This isn’t care. It’s performative liberalism at the expense of societal integrity.
Hilary Miller
January 25, 2026 AT 10:31Water every 20 minutes. Not alone. Cool space. That’s it. No fluff. This saved lives. End of story.
Keith Helm
January 27, 2026 AT 05:52It is imperative to note that the physiological mechanisms underlying drug metabolism under hyperthermic conditions are not adequately represented in current public health frameworks. The assertion that a 25–30% dose reduction is universally applicable lacks empirical validation across diverse pharmacokinetic profiles. Further, the conflation of correlation with causation in the cited NYC data warrants rigorous peer-reviewed scrutiny before policy implementation.
Daphne Mallari - Tolentino
January 27, 2026 AT 22:25While the intent behind this piece is commendable, the tone and structure betray a troubling condescension toward the reader. The use of bullet points and colloquialisms undermines the gravity of the subject. One would expect a more scholarly approach when addressing a matter of such profound public health consequence. Moreover, the reference to microbiome alterations remains speculative at best-certainly not sufficient to warrant inclusion in clinical guidance.
Alec Amiri
January 29, 2026 AT 05:29Bro. I used to do coke in my car in July. One time I passed out. Woke up in the ER. They said my heart was doing the cha-cha. I didn’t know heat could do that. Now I chill in the AC, drink water, and take half. No drama. Just living. If you’re still doing full doses in 90° heat, you’re not a rebel-you’re a statistic waiting to happen.
Lana Kabulova
January 30, 2026 AT 02:30Wait-so if you’re on antidepressants and it’s hot, you’re more likely to OD? That’s insane. I’ve been on sertraline for 6 years and I’ve never thought about this. What if the heat makes your meds stop working and you feel worse and then you take more? That’s a death spiral. Why isn’t this on every pharmacy label? Why isn’t the FDA screaming about this? This is a national emergency and no one’s talking about it except a few people on Reddit?!!??
Chiraghuddin Qureshi
January 31, 2026 AT 19:41Bro this is 🔥🔥🔥 I’m from India and we got heatwaves every year. My cousin OD’d last summer-he was using painkillers and didn’t drink water. This article? It’s like a life manual. I’m sharing it with my whole village. 🌿💧
Kenji Gaerlan
February 2, 2026 AT 10:14who even wrote this? i mean i get it but like why so many words? its just drink water dont do alone and chill. why the hell is there a whole section on gut bacteria? who cares? just tell me what to do. also i think they misspelled ‘naloxone’ like 3 times.
Oren Prettyman
February 2, 2026 AT 22:56It is worth noting that the entire premise of this article is predicated on an implicit assumption that drug use is a neutral or even benign activity requiring merely environmental mitigation. This is a dangerous fallacy. The data presented, while statistically significant in certain localized contexts, fails to account for confounding variables such as socioeconomic status, access to healthcare, and the prevalence of polypharmacy among the populations under study. Furthermore, the assertion that harm reduction is a sufficient policy response neglects the fundamental ethical imperative to address the root causes of substance use disorder through rehabilitation, not accommodation. In essence, this document does not save lives-it delays accountability.
Ryan Riesterer
February 3, 2026 AT 04:13The thermal modulation of hepatic CYP450 enzymes and renal clearance rates under hyperthermic conditions is well-documented in pharmacokinetic literature. The 25–30% dose reduction heuristic aligns with in vivo models from the 2020 JAMA Pharmacology study on thermoregulatory drug metabolism. However, the operationalization of this metric in non-clinical settings remains fraught with variability due to individual thermotolerance thresholds and hydration kinetics. The water protocol is empirically sound, but its scalability is questionable without standardized biomonitoring tools.
Akriti Jain
February 4, 2026 AT 23:21So… this is all just a cover for the government to track us? 😏 Cooling kits? With ‘overdose cards’? That’s just a QR code that logs your location and drug use. And the ‘check-in programs’? They’re sending drones with cameras to watch people use. This is how they build the database for the next phase of the War on Drugs. 🤫👁️🗨️💧
Mike P
February 5, 2026 AT 14:27Y’all act like this is some new discovery. My grandpa used to say ‘if you’re hot and high, you’re one step from dead’ back in ’78. We didn’t need a 3000-word essay. We had common sense. Drink water. Don’t use alone. Don’t be an idiot. This country’s gone soft. We used to just say ‘you made your bed, lie in it.’ Now we hand out misting bottles like it’s a damn spa day. I get it, I do. But let’s not pretend this isn’t just a fancy way of saying ‘we don’t want to see you die on the sidewalk.’ Fine. But don’t act like you’re saving the world. You’re just cleaning up after people who refused to stop.