Antihistamine Safety Checker
Check if medications contain dangerous anticholinergic ingredients commonly found in over-the-counter allergy and sleep aids.
Enter a medication name to check its safety for elderly patients.
Common Hidden Sources
Many products contain dangerous antihistamines. Check these active ingredients:
- Diphenhydramine
- Doxylamine
- Chlorpheniramine
- Hydroxyzine
- Dimenhydrinate
Products to avoid: Tylenol PM, Advil PM, NyQuil, Unisom SleepTabs, store-brand sleep aids
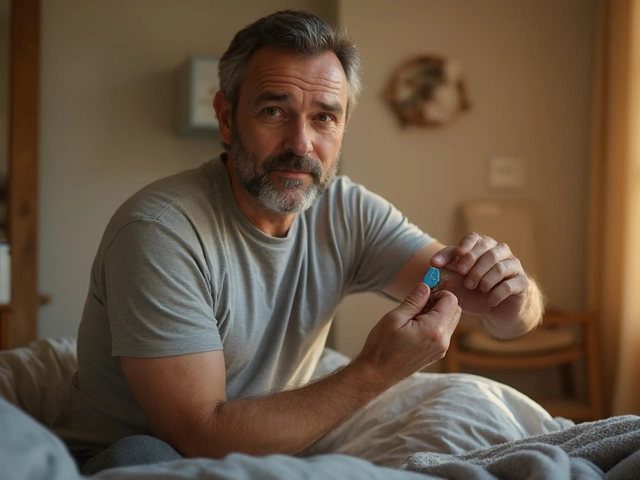
Every year, millions of older adults reach for over-the-counter sleep aids or allergy pills containing diphenhydramine or doxylamine-commonly sold as Benadryl or Unisom. They think they’re doing something simple: getting a good night’s sleep or calming a runny nose. But for people over 65, these medications aren’t harmless. They’re a quiet, widespread danger that can lead to confusion, falls, hospital visits, and even long-term cognitive decline.
Why First-Generation Antihistamines Are Risky for Seniors
First-generation antihistamines like diphenhydramine, chlorpheniramine, and doxylamine were developed in the 1940s. They work by blocking histamine, the chemical that triggers allergy symptoms. But they also block another key brain chemical: acetylcholine. This is called an anticholinergic effect. In younger people, the body handles this just fine. In older adults, it’s a different story. As we age, our brains naturally produce less acetylcholine. This neurotransmitter helps with memory, focus, and muscle control. When a medication like Benadryl blocks what’s left, it’s like turning off the last few lights in a dim room. The result? Dizziness, blurred vision, dry mouth, constipation, urinary retention, and-most dangerously-confusion and disorientation. A 2018 review of five major studies found that elderly patients taking first-generation antihistamines had more than double the risk of serious falls or fractures. That’s not a small increase. It’s a major safety threat. One fall can mean a broken hip, months in rehab, loss of independence, or worse.Confusion Isn’t Just ‘Getting Older’
Many families mistake sudden confusion in an elderly parent as just part of aging. But when someone who’s usually sharp suddenly doesn’t recognize their own home, starts talking nonsense, or tries to pack their bags to ‘go home’-even when they’re already there-that’s not normal aging. That’s anticholinergic delirium. Caregivers on forums like AARP’s community report these episodes all the time. One woman described her 78-year-old mother becoming so confused after taking Benadryl for allergies that she insisted they were in a hotel and needed to check out. Another shared that her father, who’d always been calm, started yelling at the walls after using a nighttime cold medicine. Both cases cleared up within days after stopping the medication. These aren’t rare stories. Nurses in geriatric units say they see at least two cases per month. The symptoms often mimic dementia, leading to unnecessary tests and misdiagnoses. The real fix? Stop the drug. That’s it.Second-Generation Antihistamines Are the Safer Choice
There’s a better option. Second-generation antihistamines-like cetirizine (Zyrtec), loratadine (Claritin), and fexofenadine (Allegra)-were designed differently. They’re built with polar molecules that can’t easily cross the blood-brain barrier. That means they block histamine in your nose and throat without messing with your brain. Studies show these drugs don’t increase fall risk. They don’t cause confusion. They don’t trigger delirium. In fact, the American Academy of Allergy, Asthma & Immunology explicitly recommends them for older adults. Loratadine (10 mg daily) and cetirizine (5 mg daily) are both effective for allergies and sleep issues (though cetirizine can still cause mild drowsiness in some). Fexofenadine (60 mg twice daily) is even less likely to cause sedation. None of them carry the same anticholinergic burden as Benadryl. Yes, some people say first-generation drugs work better for sleep. But that’s because they knock you out. That’s not restful sleep-it’s drug-induced sedation. And the next day? You’re groggy, unsteady, and at risk. Second-generation options don’t give you that trade-off.
Hidden Sources of Danger
The biggest problem isn’t just the allergy pills. It’s the hidden antihistamines in other over-the-counter products. Many nighttime pain relievers, cold medicines, and sleep aids contain diphenhydramine or doxylamine-and they don’t always say ‘Benadryl’ on the label. Check the active ingredients list. If you see any of these, put the bottle down:- Diphenhydramine
- Doxylamine
- Chlorpheniramine
- Hydroxyzine
- Dimenhydrinate
What Experts Say: The Beers Criteria and Beyond
The American Geriatrics Society has been warning about this since 1991. Their Beers Criteria-a trusted guide for safe prescribing in older adults-lists first-generation antihistamines as ‘potentially inappropriate medications’ for people over 65. The 2019 update called them ‘high-risk’ due to their strong anticholinergic effects. Healthcare systems are starting to respond. Medicare and Medicaid now track anticholinergic use in nursing homes. Facilities with more than 5% of residents on these drugs get lower quality ratings. That’s pushing pharmacies and doctors to review medications more carefully. But change is slow. As of 2023, over one-third of adults 65+ still regularly use first-generation antihistamines. Nearly 1 in 5 use them daily. That’s 10 million people in the U.S. alone-many of them unaware of the danger.
What to Do Instead
If you or a loved one is using Benadryl or a similar product, here’s what to do:- Check all medicine labels. Look for the active ingredients listed above.
- Switch to a second-generation antihistamine. Claritin, Zyrtec, or Allegra are safe alternatives.
- Try non-drug options. For allergies, use saline nasal sprays, HEPA filters, or allergen-proof pillowcases. For sleep, focus on sleep hygiene: cool, dark room; no screens before bed; consistent bedtime.
- Talk to a doctor or pharmacist. Ask for a full medication review. Many older adults take 5+ medications. Antihistamines can interact with antidepressants, bladder meds, and heart drugs, making side effects worse.
The Bigger Picture: Preventing Falls and Dementia
This isn’t just about one pill. It’s about protecting brain health. A 2015 study in JAMA Internal Medicine followed 800 older adults for seven years. Those who took strong anticholinergic drugs for three years or more had a 54% higher risk of developing dementia. That’s not a small risk. That’s a life-altering one. Experts estimate that eliminating first-generation antihistamines in older adults could prevent 250,000 falls and 50,000 dementia cases every year in the U.S. That’s not science fiction. It’s a direct result of stopping something that’s easy to fix.Final Thought: Safer Choices Are Simple
You don’t need a complicated plan. You don’t need expensive treatments. You just need to stop using the wrong medicine and swap it for a safer one. Benadryl isn’t a harmless sleep aid for seniors. It’s a hidden hazard. Claritin or Zyrtec isn’t just ‘another option’-it’s the standard of care. If you’re caring for an older adult, check their medicine cabinet today. If you’re over 65 and taking something for sleep or allergies, ask your pharmacist: ‘Is this safe for someone my age?’ The answer might save their independence-or even their life.Are antihistamines safe for elderly people?
Second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) are generally safe for elderly patients. First-generation antihistamines like diphenhydramine (Benadryl) and doxylamine (Unisom) are not safe. They cross into the brain, block acetylcholine, and can cause confusion, dizziness, falls, urinary retention, and even increase dementia risk.
Why is Benadryl dangerous for seniors?
Benadryl contains diphenhydramine, a first-generation antihistamine with strong anticholinergic effects. As people age, their brains produce less acetylcholine, a chemical needed for memory and coordination. Blocking what’s left can cause sudden confusion, drowsiness, low blood pressure, and impaired balance-leading to falls, fractures, or hospitalization. Even low doses can trigger these effects.
What are the signs of anticholinergic toxicity in older adults?
Signs include sudden confusion or disorientation, hallucinations, dry mouth, difficulty urinating, constipation, blurred vision, rapid heartbeat, flushed skin, and extreme drowsiness. These symptoms often appear within hours of taking the medication and can be mistaken for dementia or stroke. Stopping the drug usually reverses symptoms within 1-3 days.
Can I switch from Benadryl to Zyrtec for sleep?
Zyrtec (cetirizine) can cause mild drowsiness in some people, but it’s not designed as a sleep aid. It’s an allergy medication. For sleep, better options include melatonin (at low doses), improving sleep hygiene, or talking to a doctor about non-drug approaches. Never use antihistamines long-term for sleep-regardless of generation. They disrupt natural sleep cycles and can worsen cognitive decline.
What over-the-counter products contain dangerous antihistamines?
Common products include Tylenol PM, Advil PM, NyQuil, Aleve PM, Unisom SleepTabs, and many store-brand ‘nighttime’ cold and allergy remedies. Always check the active ingredients list. If you see diphenhydramine, doxylamine, chlorpheniramine, or hydroxyzine, avoid them. Look for products labeled ‘non-drowsy’ or ‘second-generation’ instead.
Is there a long-term risk of dementia from antihistamines?
Yes. A seven-year study in JAMA Internal Medicine found that people who took strong anticholinergic drugs-including first-generation antihistamines-for three years or more had a 54% higher risk of developing dementia compared to those who used them for three months or less. The risk increases with dose and duration. Stopping these drugs may reduce future risk, but long-term use should be avoided entirely in older adults.
What should I do if my elderly parent is already taking Benadryl daily?
Don’t stop abruptly without talking to a doctor, especially if it’s been used long-term. Schedule a medication review with their pharmacist or primary care provider. Switch to a second-generation antihistamine like loratadine for allergies, or explore non-drug solutions for sleep. Monitor for changes in confusion, balance, or urination. If symptoms appear after taking the drug, stop it immediately and seek medical advice.






14 Comments
Paul Taylor
January 26, 2026 AT 17:31Been a nurse for 32 years and I can tell you this is 100% true. I’ve seen grandmas on Benadryl for sleep go from sharp as a tack to lost in their own living room in under 48 hours. No exaggeration. Their families think it’s just aging but it’s the meds. We’ve had to pull them off these things and watch them come back to life. It’s like flipping a switch. And nobody talks about it. Why? Because it’s OTC. Nobody thinks a little purple pill could do this. But it does. And it’s killing independence one confused night at a time.
Switch to Zyrtec. It’s not magic but it’s safe. And if they’re using Tylenol PM? Throw it out. That’s Benadryl in disguise. Check the label. Always. No exceptions.
Desaundrea Morton-Pusey
January 28, 2026 AT 05:16Wow another anti-Benadryl rant. Can we just admit that Big Pharma is pushing second-gen drugs because they’re more expensive? My grandma takes Benadryl and she’s fine. She sleeps better, doesn’t fall, and isn’t hallucinating. Maybe it’s not the drug, it’s the people who can’t use it right. Stop scaring seniors into buying expensive alternatives. Benadryl’s been around since 1946. If it was that dangerous, it’d be banned.
Murphy Game
January 29, 2026 AT 09:57They don’t want you to know this but the FDA knew about the anticholinergic risks since the 80s. They buried it. Why? Because the drug companies fund their studies. Look at the Beers Criteria. It’s been updated every few years and they keep it on the list. That’s not coincidence. That’s cover-up. And now they’re pushing Zyrtec like it’s a miracle cure. But Zyrtec? It’s still a drug. And drugs are never neutral. Someone’s making money off your fear. The real solution? Stop taking everything. Let your body heal. Natural remedies. Diet. Sleep hygiene. Not another pill. This whole system is rigged.
John O'Brien
January 29, 2026 AT 12:52Bro this is the most important post I’ve read all year. My dad was on Unisom every night for 5 years. Started forgetting birthdays, walking into walls, peeing his pants. We thought it was dementia. Turned out it was just the damn sleep aid. We switched him to Claritin and he’s been lucid for 8 months. I’m telling everyone. This isn’t medical advice. This is survival. If you’re over 65 and taking anything with ‘PM’ in the name, stop. Now. Go check your cabinet. I’ll wait.
And if your pharmacist says it’s fine? Find a new pharmacist. They’re paid to sell, not save lives.
Kegan Powell
January 31, 2026 AT 11:37Life is so much simpler when you stop blaming the medicine and start blaming the system 🌱
Why do we keep thinking the answer is another pill? We’re scared of aging so we numb it. We’re scared of insomnia so we drug it. We’re scared of allergies so we chemically blind ourselves. But the truth? Our bodies are trying to tell us something. Maybe it’s not about finding a safer antihistamine… maybe it’s about finding a safer way to live.
Zyrtec is better than Benadryl? Sure. But what if the real fix is a humidifier? A warm bath? A quiet room? Less screens? Less stress? Less fear?
We’re so focused on fixing the symptom we forget to heal the soul. And that’s the real tragedy.
Love you all. Be gentle with yourselves and your elders. ❤️
April Williams
February 1, 2026 AT 06:06How is this even a debate? You’re literally choosing between dementia and a little drowsiness. If you’re still using Benadryl after reading this, you’re not just irresponsible-you’re a danger to your family. My aunt had a stroke after falling because of Unisom. She’s in a nursing home now because someone thought ‘it’s just an OTC pill.’ No. It’s a chemical lobotomy with a side of constipation. Stop being lazy. Check the label. Swap it. Do it for your parents. Do it for your future self.
Harry Henderson
February 2, 2026 AT 23:15THIS IS A CALL TO ARMS. If you’re over 65 and still taking Benadryl, you’re playing Russian roulette with your brain. This isn’t opinion. This is data. This is science. This is your life. Stop waiting for someone else to fix it. Go to your medicine cabinet RIGHT NOW. Find the purple bottle. Toss it. Replace it with Claritin. Do it before bed. Do it for your grandchildren. Do it because you owe yourself a clear mind. I’ve seen too many seniors lose everything because they trusted a label that said ‘gentle.’ It’s not gentle. It’s poison. Act now. Don’t wait for the fall. Don’t wait for the hospital. Do it today.
suhail ahmed
February 4, 2026 AT 05:03Bro in India we call this ‘dawa ki chhaap’ - the stamp of poison disguised as relief. My uncle took Benadryl for sleep for 12 years. One day he forgot his own wife’s name. Took him 3 weeks to come back after stopping it. We thought it was Alzheimer’s. Turns out it was just a cheap sleep aid from the roadside pharmacy. We’ve been preaching this in our community since. Every senior I know now checks labels like they’re reading a bomb manual. No more ‘just one pill.’ No more ‘it’s harmless.’ The truth? It’s not about the drug. It’s about the silence around it. We need to break that silence. Every time someone says ‘it’s just a pill,’ we need to say ‘it’s just a death sentence waiting to be triggered.’
Candice Hartley
February 6, 2026 AT 00:14My mom switched from Benadryl to Zyrtec and suddenly remembered my birthday. 😭
She cried. I cried. We didn’t even know she’d been confused until she wasn’t anymore.
Check your meds. Please.
astrid cook
February 7, 2026 AT 11:06So now we’re blaming OTC meds for dementia? What about all the other things? Sugar. Screen time. Loneliness. Lack of exercise? You’re making this too simple. Benadryl is not the villain. It’s the scapegoat. People like you want easy answers so you don’t have to face the real problem: we’ve abandoned our elders. We don’t visit. We don’t listen. We just drug them to keep them quiet. And now you’re blaming the pill instead of the neglect.
Andrew Clausen
February 8, 2026 AT 22:04Incorrect. The 2015 JAMA study did not establish causation. It showed association. Correlation ≠ causation. Also, fexofenadine is not 'less likely to cause sedation'-it is non-sedating in 98% of cases. Claritin is non-sedating in 95%. Cetirizine is sedating in ~15%. The post conflates efficacy with safety. Also, 'second-generation' is not a regulatory term-it's a pharmacological descriptor. Misleading language. Also, 'anticholinergic burden' is not a validated metric in all clinical contexts. This post is alarmist and lacks nuance.
Anjula Jyala
February 9, 2026 AT 23:13Anticholinergic load is quantified via ACB scale and the cumulative dose threshold for cognitive risk is >100 ACB points annually. First-gen antihistamines score 3 points each. Daily use of diphenhydramine yields 1095 ACB/year. That’s above the 100-point threshold for significant dementia risk. Cetirizine and loratadine score 0. Fexofenadine 0. The Beers Criteria is evidence-based. Your grandmother’s anecdote doesn’t override meta-analyses. Also, non-pharmacological sleep interventions have Level A evidence per AASM. You’re conflating preference with safety. This is basic geriatric pharmacology. If you don’t understand this, consult a clinical pharmacist. Don’t self-diagnose with Reddit.
Kirstin Santiago
February 11, 2026 AT 19:19I just showed this to my 82-year-old dad. He said, 'I didn’t realize Benadryl was doing this to me.' He’s been taking it since his wife passed. He thought it helped him sleep through the grief.
We switched him to Zyrtec last week. He’s been sleeping better, talking more, and even started gardening again.
It’s not magic. It’s just… not poison.
Thank you for writing this.
Kathy McDaniel
February 13, 2026 AT 10:10my grandma took benadryl for years and she’s 90 and still plays bingo every thursday 😊
maybe it’s not for everyone? idk just saying