Millions of people reach for antihistamines and decongestants every fall and spring, thinking they’re just grabbing a quick fix for a stuffy nose or itchy eyes. But these common over-the-counter meds aren’t harmless snacks. They’re powerful drugs with real, sometimes serious, risks - and most people have no idea.
What You’re Actually Taking
Antihistamines like diphenhydramine (Benadryl) and loratadine (Claritin) block histamine, the chemical your body releases during an allergic reaction. That stops sneezing, runny nose, and itching. But first-gen antihistamines - the ones you find in sleep aids and cheap cold meds - don’t just stop histamine in your nose. They cross into your brain. That’s why 60% of people who take diphenhydramine feel drowsy. Some feel dizzy. Others get blurry vision or dry mouth. It’s not just annoying - it’s dangerous. Decongestants like pseudoephedrine (Sudafed) and phenylephrine work differently. They shrink swollen blood vessels in your nasal passages. That’s why your nose clears up fast. But those same blood vessels are everywhere - in your heart, your brain, your kidneys. When you constrict them in your nose, you’re also tightening them elsewhere. That’s why your heart races, your blood pressure spikes, and you can’t sleep.The Hidden Dangers of First-Generation Antihistamines
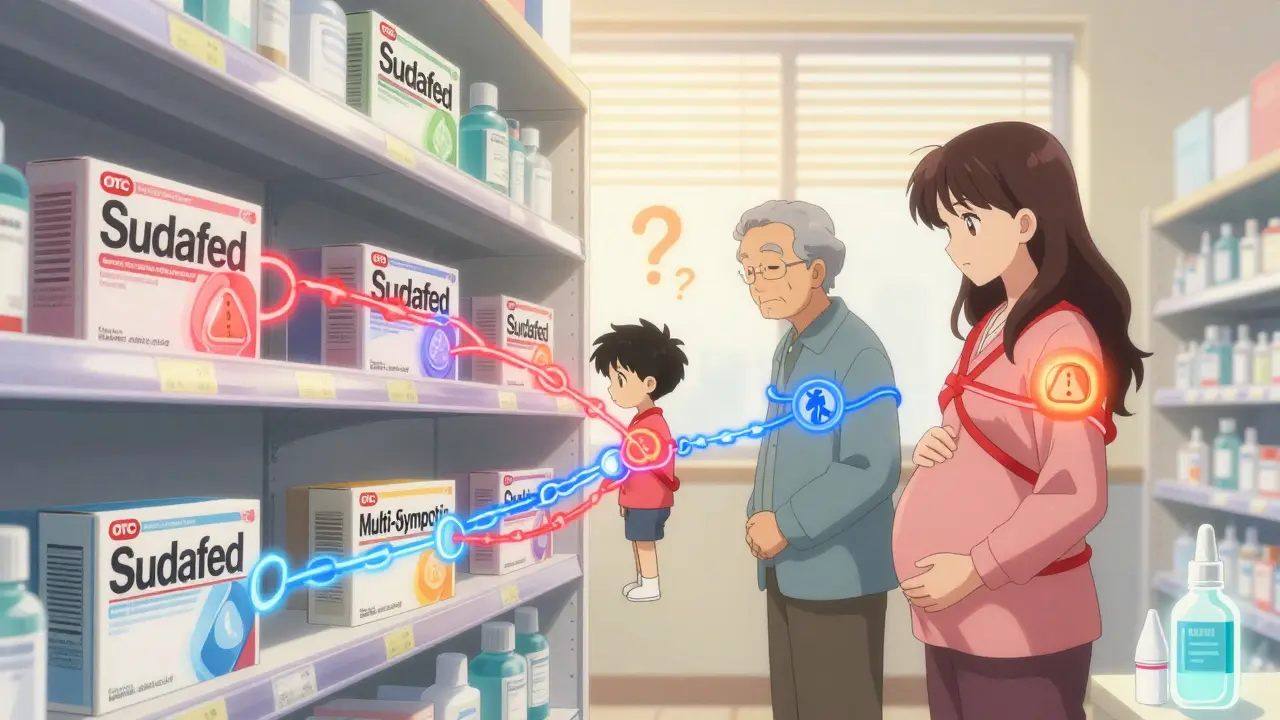
If you’re over 65, taking Benadryl for allergies might be one of the riskiest things you do every day. The American Geriatrics Society calls first-gen antihistamines potentially inappropriate for older adults. Why? Because they have strong anticholinergic effects - meaning they block a key brain chemical called acetylcholine. That’s fine if you’re trying to sleep. Not fine if you’re trying to remember where you put your keys. Studies show older adults on these meds have a 300% higher risk of falling. That’s not a typo. One fall can mean a broken hip, a hospital stay, and a lifetime of reduced mobility. They also cause confusion, urinary retention (especially dangerous for men with enlarged prostates), and can make glaucoma worse. AARP found that many seniors on these meds develop anxiety, constipation, and trouble peeing - symptoms they blame on aging, not their medicine. Even younger people aren’t safe. Mixing diphenhydramine with alcohol or sleep aids can slow your breathing to dangerous levels. Combine it with an antidepressant, and you’re playing Russian roulette with your heart rhythm.Decongestants: The Silent Blood Pressure Killer
Pseudoephedrine doesn’t just unblock your nose - it can block your heart’s ability to relax. The Mayo Clinic says it can raise systolic blood pressure by 5 to 10 mmHg. For someone with normal blood pressure, that’s a nuisance. For the 116 million American adults with high blood pressure? That’s a medical emergency waiting to happen. And it’s not just the pills. Nasal sprays like Afrin (oxymetazoline) seem safer because they’re local. But use them for more than three days? You’re almost guaranteed to get rebound congestion - your nose gets worse than before. Half of users develop this cycle. Then they use more spray. Then they get addicted. Then they need a doctor to break the habit. Phenylephrine, the ingredient now in most Sudafed products, was pulled from OTC sale in Europe in 2022 because studies showed it doesn’t even work well. But in the U.S., it’s still everywhere. And it still raises blood pressure - just less predictably. That makes it more dangerous, not less.
Combination Products: The Overdose Trap
You think you’re buying one thing - a cold and allergy pill. But 68% of these products contain multiple active ingredients. One pill might have an antihistamine, a decongestant, and acetaminophen (Tylenol). That sounds efficient. Until you take another Tylenol for a headache. Or drink a soda with caffeine. Or take your blood pressure med. Acetaminophen is the leading cause of acute liver failure in the U.S. The safe daily limit is 4,000 mg. But many people don’t realize that one “all-in-one” cold tablet has 500 mg. Take two of those, plus two more Tylenol, and you’re at 2,000 mg before lunch. By dinner, you’re at 4,000 mg. No warning signs. No pain. Just silent liver damage. And if you’re on an SSRI antidepressant? Taking a decongestant with it can spike your blood pressure to 180 mmHg or higher. That’s not a scare tactic - it’s documented. Emergency rooms see these cases every winter.Who Should Never Take These Meds
The NHS and FDA have clear lists. If you have:- High blood pressure
- Heart disease
- Diabetes
- Enlarged prostate
- Glaucoma
- Thyroid problems
- Liver or kidney disease
What to Do Instead
You don’t need a decongestant to breathe better. Intranasal corticosteroids like fluticasone (Flonase) or mometasone (Nasonex) are more effective for chronic congestion - and they don’t raise your blood pressure. They take a few days to work, but they’re safe for long-term use. For allergies, saline nasal rinses (Neti pots) clear out pollen and irritants without drugs. Cold compresses reduce swelling. A humidifier helps. And if your symptoms last more than 10 days? You don’t have allergies - you might have a sinus infection. Antihistamines can make that worse by thickening mucus.When to Talk to a Pharmacist or Doctor
Most people never do. But 78% of OTC allergy medication problems could be avoided with a quick chat with a pharmacist. They know what’s in your cabinet. They know what you’re taking for your blood pressure. They know which meds interact dangerously with caffeine or energy drinks. If you’re over 65, don’t use any first-gen antihistamine without asking. If you’re on any prescription med, check for interactions before buying anything labeled “allergy” or “cold.” If your child is under 2 - don’t give them anything without a doctor’s order. The FDA has documented deaths from these products in babies.The Bottom Line
Allergy meds aren’t candy. They’re powerful tools - and like any tool, they can hurt you if you don’t use them right. The fact that you can buy them without a prescription doesn’t mean they’re safe. It means you have to be smarter about using them. Don’t assume “natural” or “non-drowsy” means harmless. Don’t think “it’s just for a few days” - rebound congestion and blood pressure spikes don’t care how long you’ve used it. And don’t ignore your body’s warning signs: racing heart, dizziness, confusion, trouble peeing, or worsening congestion after three days. If your allergies are bad enough to need daily meds, talk to an allergist. There are better, safer options. And if you’ve been popping antihistamines for years because “it’s just what I’ve always done”? It’s time to rethink that.Can I take antihistamines every day for allergies?
Second-generation antihistamines like loratadine, cetirizine, or fexofenadine are generally safe for daily use in adults. They’re non-sedating and don’t cause tolerance. But first-gen ones like diphenhydramine should never be used daily - they build up in your system, increase fall risk, and can damage your brain over time. If you need daily meds, see an allergist. There are better long-term options like nasal steroids.
Is pseudoephedrine safer than phenylephrine?
Pseudoephedrine works better and has more predictable effects. Phenylephrine, which replaced it in most OTC products, has weak evidence of effectiveness and still raises blood pressure. Neither is safe for people with high blood pressure or heart conditions. If you need a decongestant, use it for no more than three days - and only if your doctor says it’s okay for you.
Why do some allergy meds make me feel wired or anxious?
That’s the decongestant kicking in. Pseudoephedrine and phenylephrine stimulate your nervous system, increasing adrenaline. That’s why you feel alert, jittery, or have a racing heart. It’s not “just caffeine.” It’s a drug effect. If you’re sensitive to stimulants, avoid decongestants entirely. Try saline rinses or nasal steroids instead.
Can I give my 4-year-old children’s Benadryl for allergies?
Never give diphenhydramine to a child under 6 without a doctor’s direction. The FDA warns against all OTC cough and cold meds for kids under 2. Even older kids can have severe reactions - seizures, rapid heartbeat, hallucinations. For children, use saline drops, a humidifier, and consult a pediatrician. Antihistamines aren’t always the right answer for kids.
Are there natural alternatives to antihistamines and decongestants?
Yes. Saline nasal irrigation (Neti pot) clears allergens without drugs. Intranasal corticosteroids like Flonase are more effective than decongestants for chronic congestion and have no systemic side effects. Quercetin, a plant flavonoid, shows promise in early studies as a natural antihistamine, but it’s not proven to replace medication. Always talk to your doctor before replacing meds with supplements.
How do I know if I’m having a bad reaction?
Call for help if you have: chest pain, fast or irregular heartbeat, severe headache, trouble breathing, confusion, hallucinations, or sudden inability to urinate. These are signs of a serious reaction - not just side effects. Don’t wait. Go to the ER or call poison control. OTC doesn’t mean safe.
Why does my nose get worse after using Afrin for a week?
That’s called rebound congestion. The spray shrinks blood vessels in your nose. When it wears off, they swell back even bigger. After 3 days, your body gets dependent. You need more spray to feel clear. The only fix is to stop using it - which is hard because your nose gets worse before it gets better. See a doctor for a plan to wean off safely. Nasal steroids help during recovery.
Can I take allergy meds with my blood pressure pills?
Decongestants like pseudoephedrine can make your blood pressure meds less effective or cause dangerous spikes. Even second-gen antihistamines can interact with some heart meds. Always check with your pharmacist before combining any OTC allergy med with your prescription drugs. There’s no such thing as a “safe” combo without knowing your full medication list.
If you’ve been using these meds for years without thinking twice, you’re not alone. But now you know the risks. The next time you reach for that bottle, ask yourself: Is this helping me - or just masking a problem that needs real care?





14 Comments
Jody Patrick
December 17, 2025 AT 06:21These meds are a scam. Big Pharma wants you hooked. They don’t care if you fall or have a stroke - as long as you keep buying.
Stop trusting the label. Read the fine print. Or keep being a sheep.
Jigar shah
December 18, 2025 AT 07:36The pharmacokinetics of first-generation antihistamines are particularly concerning in elderly populations due to reduced hepatic clearance and increased blood-brain barrier permeability.
Acetylcholine antagonism leads to cognitive impairment that mimics early-stage dementia - a misdiagnosis trap many clinicians overlook.
Sachin Bhorde
December 19, 2025 AT 16:37Yo, this is wild but so true.
I used to pop Benadryl like candy to sleep - turned out my brain was on pause for 3 years.
Switched to Zyrtec and a humidifier - no more foggy mornings.
Also, Neti pot changed my life. No more nose junk.
Stop the meds, start the rinse.
Trust me, bro.
Also, phenylephrine? Total scam. Why’s it still here? 🤦♂️
Joe Bartlett
December 21, 2025 AT 14:38British people don’t even use these. We use steam and salt water.
Simple. Safe. Works.
Why do Americans need a pill for everything?
Just breathe.
Marie Mee
December 23, 2025 AT 06:35They're putting this in everything now... I swear the government wants us confused and sick
They don't want us healthy
Look at the labels they hide the truth
Big Pharma owns the FDA
They're poisoning us slowly
Why do you think everyone's so tired?
It's the meds
It's the chemicals
It's all connected
I stopped taking everything
I'm fine now
They don't want you to know this
Naomi Lopez
December 24, 2025 AT 20:01It’s astonishing how little public health literacy exists around OTC pharmacology.
These aren’t ‘medicines’ - they’re neuroactive compounds with off-target effects that are statistically correlated with geriatric decline, cardiovascular events, and iatrogenic dependency.
And yet, we treat them like aspirin.
Chilling.
Salome Perez
December 25, 2025 AT 20:14As someone who grew up in Mumbai with seasonal allergies, I never used pills until I moved to the U.S.
Here, everyone reaches for a bottle like it’s water.
Back home? We used tulsi leaves, steam with eucalyptus, and a cloth over the nose.
It’s not magic - it’s tradition.
And it works.
Maybe we’ve forgotten how to heal without chemicals.
Not saying pills are evil - just that we’ve lost balance.
Ask your grandma. She probably knows better.
Kent Peterson
December 26, 2025 AT 04:44I’ve read this article three times. And I still think it’s overblown. Seriously? You’re telling me that people who take Claritin for 20 years are at risk? That’s not science - that’s fearmongering. The data is weak. The risks are minuscule compared to, say, eating processed food. And don’t get me started on the ‘rebound congestion’ myth - that’s not even a real diagnosis in most countries! Also, why are you blaming phenylephrine? It’s been studied. It works. It’s just slower. And yes, I’ve used Sudafed for 15 years. My blood pressure? Perfect. So stop scaring people with cherry-picked stats. #NotAllOfUsAreFools
Josh Potter
December 26, 2025 AT 17:30Bro I was addicted to Afrin for 4 years.
Woke up every morning like I was suffocating.
Went to a doc - they gave me Flonase and told me to quit cold turkey.
First 3 days? Worst nasal pain of my life.
Day 5? I could breathe again.
Now I use a neti pot every morning.
Best decision ever.
Stop the spray. Start the water.
You’ll thank me later.
Evelyn Vélez Mejía
December 27, 2025 AT 09:05There is a profound cultural pathology at play here: the commodification of comfort.
We have outsourced our bodily wisdom to chemical solutions, mistaking suppression for healing.
Antihistamines and decongestants are not treatments - they are distractions from environmental degradation, poor indoor air quality, and systemic neglect of preventative care.
When we treat symptoms as the enemy, we become dependent on the machinery that manufactures them.
This is not pharmacology - it is a symptom of a civilization that has forgotten how to listen to its own body.
Jane Wei
December 28, 2025 AT 15:37I just started using Flonase last year. Took a month to notice a difference. But now I don’t even think about my allergies.
Worth the wait.
Also, no more 3 p.m. naps.
Life’s good.
Radhika M
December 28, 2025 AT 17:55My mom in India takes neem leaves with honey for allergies. No side effects. Works better than pills.
People forget: nature gave us solutions before Big Pharma existed.
Try it. Safe. Cheap.
And no weird heart racing.
Philippa Skiadopoulou
December 29, 2025 AT 01:09Decongestants remain contraindicated in patients with uncontrolled hypertension, regardless of formulation.
Phenylephrine’s efficacy is questionable, yet its safety profile remains clinically significant.
Pharmacists must be proactive in screening for polypharmacy risks.
Simple advice: consult before purchase.
Pawan Chaudhary
December 29, 2025 AT 04:16My cousin took Benadryl every night for insomnia. Thought it was harmless.
Turned out he had memory loss, urinary issues, and fell twice.
Doctor said it was all from the meds.
Now he uses melatonin and a fan.
Best sleep of his life.
Don’t be like him. Ask first.