Why the Difference Between Extended-Release and Immediate-Release Medications Can Save Your Life
You take your medication like clockwork. Every morning. No skipping. But sometimes, you don’t feel anything for hours. Other times, you feel too much-too fast. That’s not just in your head. It’s the difference between extended-release and immediate-release drugs.
These aren’t just different brands. They’re completely different systems. One releases the drug slowly over 12 to 24 hours. The other dumps it all into your system in 30 minutes. Get it wrong, and you risk side effects, overdose, or no relief at all. This isn’t theory. It’s real. People end up in emergency rooms because they crushed a pill they thought was just a tablet. Others take extra doses because they didn’t feel the effect fast enough-and didn’t know it was supposed to take days to build up.
Understanding how these two types work isn’t just helpful. It’s necessary for safety.
How Immediate-Release Medications Work
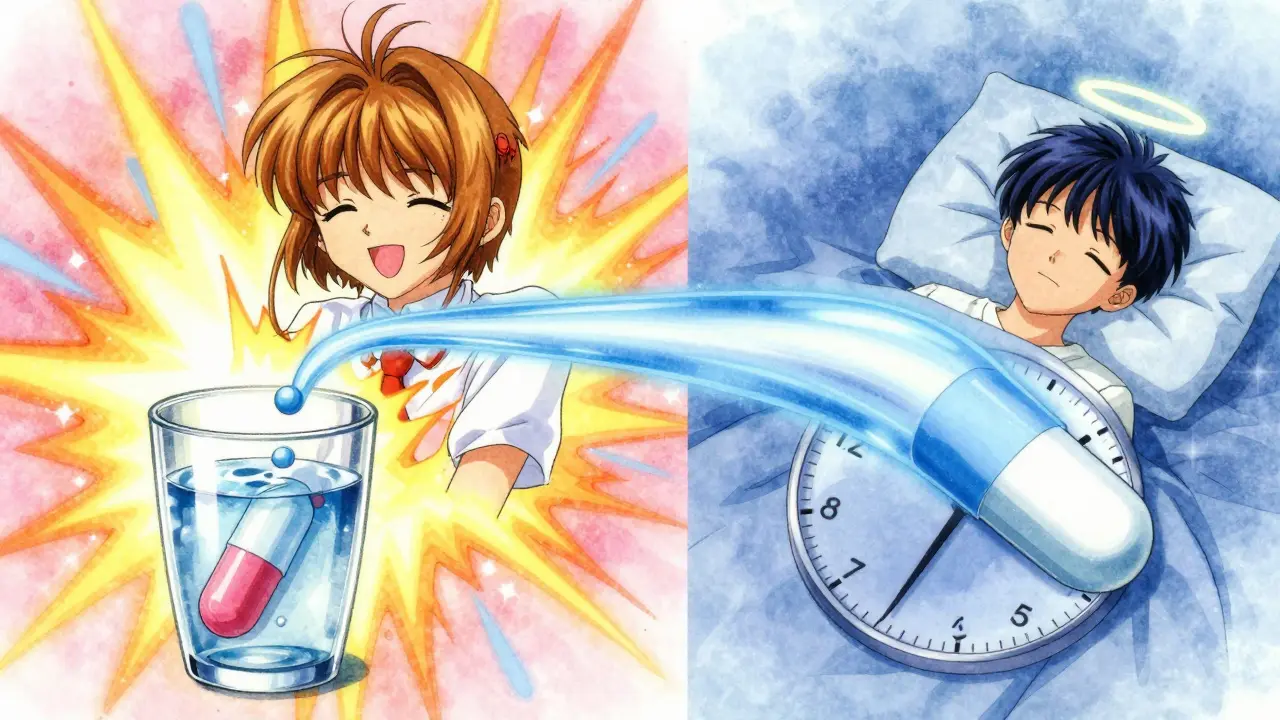
Immediate-release (IR) pills are the classic kind. You swallow them, and within 15 to 30 minutes, the drug starts dissolving. Peak levels hit your bloodstream in 30 to 90 minutes. That’s why IR painkillers like oxycodone or ibuprofen make you feel relief so quickly. Same with IR ADHD meds like Adderall IR or IR antidepressants like sertraline.
The upside? Fast action. If you’re having a panic attack, a breakthrough pain flare, or need to focus for a presentation, IR gives you control. You take it when you need it. You feel it when you need it.
The downside? The ride is bumpy. Your blood levels spike high, then drop fast. That’s why people on IR Adderall often crash by mid-afternoon. Or why IR metoprolol can cause sudden dizziness when levels drop too low. These peaks and valleys stress your body. They’re harder on your liver and kidneys. And they make it easier to accidentally take too much.
Take bupropion, for example. The IR version can push blood levels above 400 ng/mL within two hours. The seizure threshold? Around 350 ng/mL. That’s why IR bupropion is dosed in smaller amounts, multiple times a day. One big IR dose? Dangerous. That’s why ER versions exist.
How Extended-Release Medications Work
Extended-release (ER), also called XR, SR, or CR, is designed to be steady. No spikes. No crashes. These pills use clever tech: gels that swell and slowly release the drug, tiny pellets coated to dissolve at different times, or osmotic pumps that push the medicine out like a slow drip.
Take Concerta for ADHD. It uses an osmotic pump. Water flows in, pressure builds, and the drug leaks out over 12 hours. No chewing. No crushing. No splitting. Break that system, and you get the whole dose at once. That’s how someone ends up with a seizure after swallowing a crushed tablet.
ER versions of antidepressants like sertraline or venlafaxine keep blood levels steady between 100 and 200 ng/mL all day. That’s why patients report fewer side effects-less nausea, less jitteriness, better sleep. Studies show ER users are 22% more likely to stick with their meds long-term. That’s huge for conditions like hypertension or depression, where consistency matters more than speed.
But ER isn’t magic. It takes time. You won’t feel it the first day. It can take 7 to 10 days to reach full effect, compared to 3 to 5 for IR. That’s why so many people think it’s not working and double up. And that’s when trouble starts.
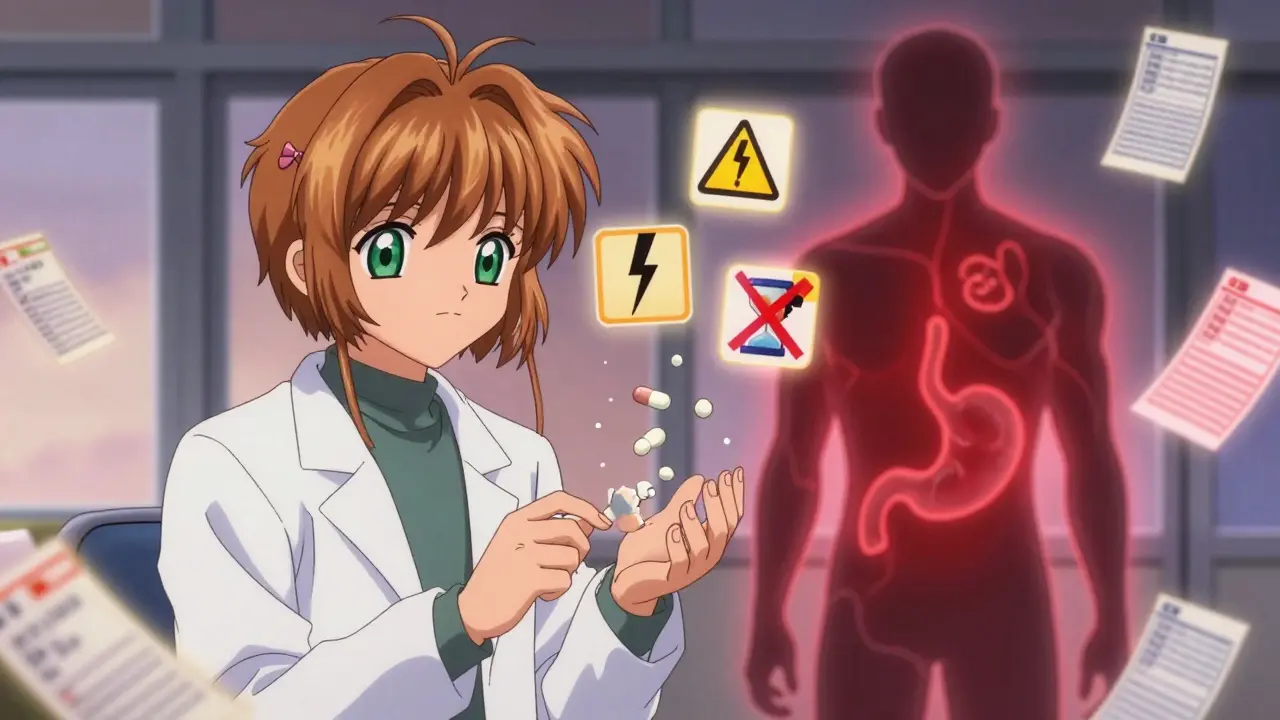
The Risks of Misusing Extended-Release Medications
Here’s the scary part: 92% of ER medications are not safe to crush, chew, or split. Yet, people do it all the time.
Why? Because they’re frustrated. They don’t feel it fast enough. Or they can’t swallow the big pill. Or they think, “It’s just medicine-what’s the difference?”
The FDA has issued warnings about this for years. Crushed ER opioids like OxyContin or ER morphine can deliver a full lethal dose in minutes. ER bupropion? Crushed, it can cause seizures. ER metformin? Crushed, it can cause dangerous spikes in blood sugar.
Pharmacists in Halifax report that 23% of ER-related medication errors come from people splitting tablets. Venlafaxine XR, for example, isn’t scored. It’s not meant to be broken. But patients do it anyway-thinking they’re saving money or adjusting the dose. Instead, they’re risking overdose.
And if you have gastroparesis-where your stomach empties slowly-the ER drug can sit and build up. Your body absorbs it all at once. That’s why the FDA warned in 2023 that ER meds can be unpredictable in people with digestive delays. What’s safe for one person can be dangerous for another.
When to Choose Immediate-Release
ER isn’t always better. Sometimes, you need speed.
Think about breakthrough pain. If you’re on ER oxycodone for chronic pain but have a sudden flare, your doctor might give you IR oxycodone for rescue. Same with anxiety. If you’re on ER sertraline but have a panic attack, you might need a fast-acting benzodiazepine-IR-on hand.
Psychiatrists use IR meds for titration. Starting someone on a new antidepressant? They begin with IR to find the right dose before switching to ER. Why? Because you can adjust faster. If 50mg causes nausea, you drop to 25mg the next day. With ER, you’re stuck waiting days to see the effect.
And in emergencies? IR wins. If someone overdoses on IR, the drug is mostly gone in 6 to 8 hours. Overdose on ER? The drug keeps leaking into the bloodstream for 24 to 48 hours. That’s why ER overdose cases need longer hospital stays. The poison doesn’t stop coming.
That’s why many patients keep both. One Reddit user with ADHD said: “I use Adderall XR for work, but I keep 5mg IR tabs for presentations. I need that instant focus.” That’s smart. It’s not about one being better. It’s about using the right tool for the job.
Cost, Convenience, and Real-World Trade-Offs
ER meds usually cost 15% to 25% more than IR. Adderall XR might be $400 for 30 pills. Adderall IR? Around $320. Same active ingredient. Same total daily dose. But the ER version is more expensive because of the tech inside.
But here’s the catch: ER saves money in the long run. A 2022 JAMA study tracked 15,000 people with high blood pressure. Those on ER meds had 78% adherence. Those on IR? Only 56%. Missed doses mean more doctor visits, more ER trips, more hospitalizations. ER may cost more upfront, but it reduces total healthcare costs.
And convenience? Huge. One pill a day instead of three. No remembering to take it at lunch. No school nurses giving you pills. No coworkers asking why you’re popping pills at 2 p.m.
But don’t let cost or convenience blind you to risk. If you can’t afford ER, IR is fine-as long as you take it exactly as prescribed. And if you can afford ER, don’t assume it’s safer if you misuse it. The technology only works if you don’t break it.
What You Need to Do Right Now
Here’s your checklist:
- Look at your prescription bottle. Does it say XR, ER, SR, CR, or DR? If yes, do not crush, chew, or split it.
- Ask your pharmacist: “Is this pill safe to break?” If they hesitate, it’s not.
- If you don’t feel the effect after a day or two, don’t take more. Wait. ER takes 7 to 10 days to build up.
- If you need faster relief, ask your doctor about keeping an IR version on hand for emergencies.
- If you have stomach issues-slow digestion, gastroparesis-tell your doctor. ER meds might not be right for you.
Medications aren’t one-size-fits-all. The same pill can be a lifeline-or a danger-depending on how you use it.
Frequently Asked Questions
Can I split an extended-release pill if it’s too big to swallow?
No, unless the pill is specifically scored and labeled as safe to split. Most extended-release pills are not designed to be broken. Splitting them can destroy the slow-release mechanism and cause a dangerous surge of medication. If you have trouble swallowing pills, ask your doctor or pharmacist for a liquid version, a smaller tablet, or a different formulation.
Why does my extended-release medication take so long to work?
Extended-release medications are built to reach steady levels slowly. While immediate-release drugs peak in hours, ER versions can take 7 to 10 days to fully build up in your system. This is normal. Taking extra doses because you don’t feel it right away can lead to overdose. Be patient. The benefits come from consistency, not speed.
Is extended-release always better than immediate-release?
No. Extended-release is better for long-term, stable conditions like depression, high blood pressure, or ADHD maintenance. But immediate-release is better for sudden symptoms-breakthrough pain, panic attacks, or when adjusting doses. Many patients use both: ER for daily control and IR for emergencies. The best choice depends on your condition, lifestyle, and how your body responds.
What happens if I accidentally crush an extended-release pill?
You may get the full dose all at once. This can cause dangerous side effects, including overdose. For example, crushing ER opioids can lead to respiratory failure. Crushing ER bupropion can trigger a seizure. If you accidentally crush or chew an ER pill, contact your doctor or poison control immediately. Do not wait for symptoms to appear.
Can I switch from immediate-release to extended-release on my own?
Never. Switching between IR and ER requires medical supervision. The dosages aren’t always equal. For example, 30mg of Adderall IR taken three times a day is not the same as 30mg of Adderall XR once daily. Your doctor will adjust your dose and timing carefully to avoid side effects or withdrawal. Always consult your prescriber before changing your medication form.
Next Steps
If you’re on an extended-release medication, check your pill bottle today. Look for labels like XR, ER, SR, or CR. If you’re unsure whether it’s safe to break or crush, call your pharmacy. Don’t guess.
If you’re new to ER meds and feeling impatient, remind yourself: this isn’t a delay. It’s a design. The goal isn’t to feel it now-it’s to feel steady all day.
If you’re caring for someone who takes these medications, learn the difference. A simple mistake-crushing a pill, doubling a dose-can have life-altering consequences. Knowledge isn’t just power. It’s protection.







8 Comments
Donna Macaranas
February 2, 2026 AT 03:56I used to crush my ER metformin because the pills were huge. Didn't realize I was risking spikes until my doc sat me down. Now I just ask for the liquid. Best decision ever. No more stomach chaos.
Jamie Allan Brown
February 3, 2026 AT 18:40My grandma took her ER blood pressure pill with a smoothie because she couldn't swallow pills. The pharmacist caught it. She thought it was just 'medicine in a capsule.' Turns out, crushing ER meds is like opening a firehose in your bloodstream. Scary stuff. Glad she listened.
Lisa Rodriguez
February 5, 2026 AT 05:41Let me tell you about my ADHD journey. I was on Adderall IR for years. Crashed by 3pm, needed another dose, felt like a zombie by dinner. Switched to XR and life changed. No more midday panic, no more hiding pills at work. Took 10 days to feel the full effect but damn if it wasn't worth the wait. Also, I keep 5mg IR on hand for big presentations. That's the combo that works. Don't be afraid to ask your doc for both.
And if you think ER is 'slow acting'-it's not slow, it's steady. Like a good bassline, not a drum solo.
Lilliana Lowe
February 6, 2026 AT 04:07It's frankly astonishing how many people treat pharmaceutical formulations like they're generic candy. The very notion that one can 'just split' an osmotic tablet without understanding its mechanical design reflects a fundamental ignorance of pharmacokinetics. The FDA warnings exist for a reason-not because doctors are overcautious, but because laypersons persistently misunderstand the difference between a pill and a time-release mechanism. The fact that 23% of ER-related errors stem from splitting unscored tablets is not a statistic-it's a public health indictment.
Furthermore, the assertion that 'it's just medicine' is not only inaccurate, it's dangerously reductive. ER formulations are engineered with polymer matrices, osmotic pumps, and enteric coatings precisely to avoid peak plasma concentrations. Crushing them is not a minor oversight-it's pharmacological sabotage. And for those who claim they 'can't swallow' the pill-there are liquid alternatives, transdermal patches, even chewable IR versions. Choose wisely, or choose to suffer the consequences.
Melissa Melville
February 6, 2026 AT 07:31lol so i took my ER sertraline like a regular pill and thought it wasn’t working so i doubled it. then i spent 3 days feeling like a robot on a treadmill. my mom called me a 'pharmaceutical idiot' and i cried. now i know. ER ain’t fast. it’s chill. like a slow jam. take it easy, baby.
Deep Rank
February 7, 2026 AT 09:01okay but let me tell you something real. i been on ER bupropion for 2 years and i swear to god i think it made me more anxious at first because i was waiting for it to kick in and i kept thinking 'why am i not happy yet' and i started taking extra because i thought it was broken and then i had a panic attack in the grocery store and the cashier asked if i was okay and i just cried and said 'i think my brain is broken' and then i went to the pharmacy and the pharmacist looked at me like i was a toddler holding a grenade and said 'did you crush it?' and i said 'no but i thought about it' and she said 'you're lucky you're alive' and now i take it with my coffee and i don't touch it and i'm fine. but if you're taking it and you're not feeling it after a day you're not broken you're just impatient and that's the real problem. your brain is not broken your expectations are. and also if you have gastroparesis you should probably stop reading reddit and go see a real doctor because you're gonna die.
Naomi Walsh
February 8, 2026 AT 17:44How is it possible that in 2024, people still believe that medication is a one-size-fits-all, no-brainer affair? The very notion that 'crushing a pill is harmless' reveals a catastrophic erosion of scientific literacy. The pharmacokinetic profiles of ER formulations are not suggestions-they are engineered constraints. To violate them is not negligence; it is intellectual arrogance disguised as self-reliance. And let’s not pretend that cost is a valid excuse-insurance covers ER formulations for a reason: because the long-term morbidity and ER visits from IR misuse cost the system tenfold. This isn’t about convenience. It’s about competence. Or the lack thereof.
Bryan Coleman
February 8, 2026 AT 18:37My brother took his ER oxycodone after crushing it because he thought it'd help his back pain faster. Ended up in ICU for 4 days. They had to use naloxone. He’s fine now, but he won’t touch ER meds without a pharmacist standing next to him. I showed him this post. He said he’ll keep it on his fridge. Good. Maybe someone else will read it before they make the same mistake.