When it comes to skin cancer, melanoma is the one you can’t afford to ignore. It makes up less than 2% of all skin cancer cases, but it causes more than 80% of skin cancer deaths. The difference between life and death often comes down to one thing: when it’s found. If caught early, the 5-year survival rate is over 99%. If it spreads, that number drops to just 32.1%. That’s not a guess-it’s data from the American Cancer Society in 2025. The good news? We’re getting better at catching it early, and we’re treating advanced cases in ways that were unthinkable just a decade ago.
How Melanoma Is Found Before It Spreads
For years, the only tool doctors had was the naked eye. A suspicious mole? That’s it. But studies show primary care providers miss up to 40% of melanomas using just visual checks. The problem isn’t always lack of skill-it’s that melanoma doesn’t always look like the textbook example. Some are flat. Some are colorless. Some grow under nails or on the scalp. And they can look exactly like harmless freckles. That’s where technology is stepping in. Dermoscopy, a handheld magnifying tool with polarized light, became the gold standard in dermatology clinics. But now, AI is taking it further. Systems like SegFusion, developed at Northeastern University, combine two neural networks: one to outline the exact shape of a lesion, and another to classify it. In tests, it hits 99% accuracy. That’s not theory-it’s real data from over 12,000 dermoscopic images. The system even balances out skewed data, because melanoma is rare in most datasets, making AI models prone to ignoring it. SegFusion fixes that by artificially boosting melanoma examples in training, so the AI doesn’t overlook the needle in the haystack. Then there’s the iToBoS full-body scanner from the EU-funded project. It takes six minutes to scan a patient’s entire skin surface. The machine doesn’t just take pictures-it analyzes every spot for texture, color, and shape changes, then flags anything risky. What’s unique? It uses explainable AI (XAI). That means when it says “this spot is suspicious,” it shows the doctor exactly why-highlighting the specific patterns it saw. No black box. No guesswork. Clinics in Germany, France, and Italy are already using it. And you don’t need a dermatologist to use some of these tools. DermaSensor, approved by the FDA in January 2024, is a pen-like device that shines near-infrared light on a mole. It measures how the light scatters and absorbs-changes that happen when cells turn cancerous. Primary care doctors can use it after just 2-3 hours of training. In trials, it boosted diagnostic confidence by 87%. But here’s the catch: its specificity is only 26-40%. That means for every 100 people it flags, 60-74 don’t have melanoma. That’s a lot of unnecessary biopsies.The Wearable That Could Change Everything
What if you could check your skin at home-every day-without a doctor’s visit? That’s the goal of a wearable patch developed at Wake Forest University. It’s tiny, battery-free, and sticks to your skin like a Band-Aid. Inside, it sends a tiny electrical signal through the mole and measures how the tissue responds. Cancerous cells conduct electricity differently than healthy ones. In a small study of 10 people, the patch showed clear, statistically significant differences between benign and malignant lesions. The team is now testing conductive hydrogel electrodes to make the patch stick better and last longer. The vision? A device you wear for 24 hours, then sync to your phone. If it detects a red flag, you get a prompt to see a doctor. No more waiting for a mole to change. No more second-guessing. Just real-time monitoring. But here’s the reality check: all these tools struggle with darker skin tones. A March 2025 JAMA Dermatology study found AI models perform 12-15% worse on people with skin of color. Why? Because most training data comes from lighter-skinned populations. This isn’t a glitch-it’s a systemic flaw. Researchers are now actively recruiting diverse participants to fix it. Until then, anyone with darker skin should not rely on AI alone. Trust your eyes, your doctor, and if something feels off, get it checked.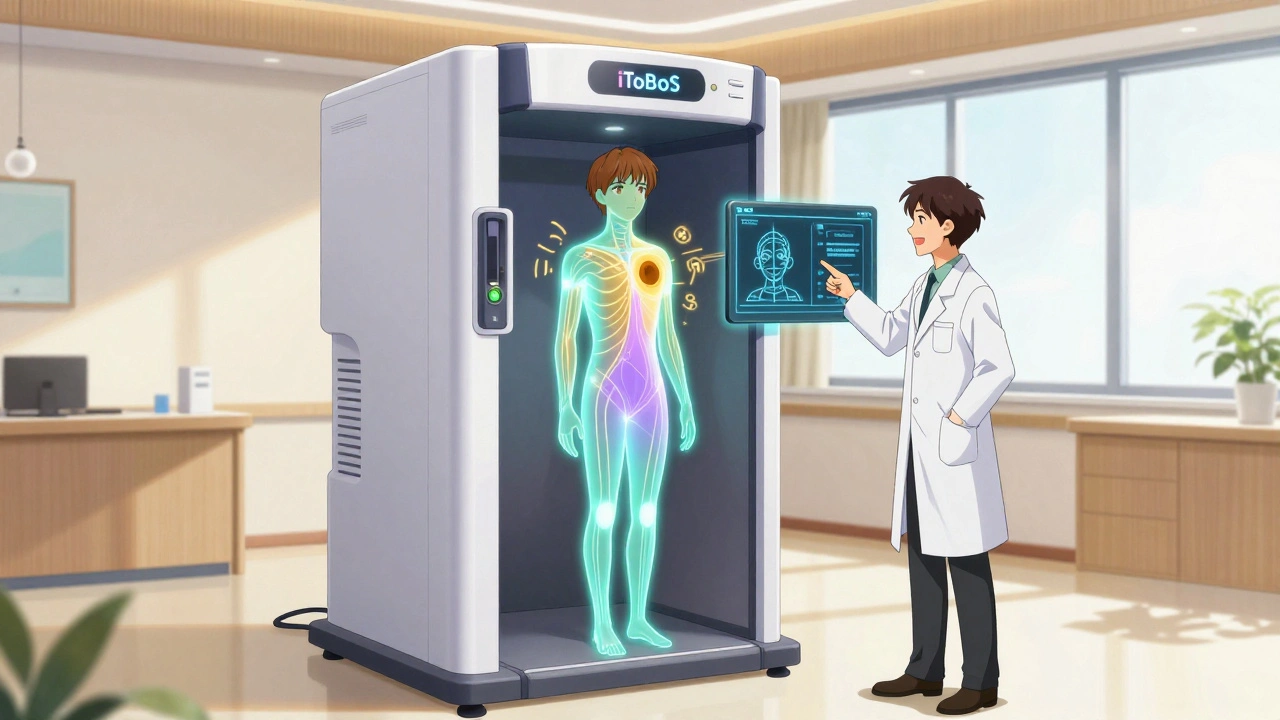
Immunotherapy: Turning the Body Into a Cancer Fighter
If melanoma spreads to lymph nodes or organs, surgery and radiation often aren’t enough. That’s where immunotherapy changed the game. Before 2011, metastatic melanoma meant months to live. Now, some patients live for years. Why? Because we stopped trying to kill cancer with chemicals and started teaching the immune system to do it. The first breakthrough was ipilimumab, approved in 2011. It blocks a protein called CTLA-4, which acts like a brake on immune cells. Letting go of that brake lets T-cells attack cancer. But it came with brutal side effects-colitis, liver damage, severe fatigue. Then came pembrolizumab and nivolumab, which block PD-1, another immune brake. These were more targeted, with fewer side effects. Today, the standard for advanced melanoma is a combo: one drug targeting PD-1, another targeting CTLA-4. Together, they double the chance of long-term survival compared to either alone. Newer drugs are on the horizon. Regeneron’s fianlimab, a LAG-3 blocker, is being tested with a PD-1 inhibitor. Early results show deeper, longer-lasting responses. Then there’s IMA203 PRAME cell therapy, currently in Phase 3 trials. It’s not a drug-it’s your own immune cells, retrained in a lab to hunt down melanoma cells with a specific marker called PRAME. In early trials, 56% of patients saw their tumors disappear completely. These aren’t miracle cures. Not everyone responds. Some tumors have ways to hide from the immune system. But for those who do respond, the results can be life-changing. One patient in a 2024 study had melanoma spread to his liver and lungs. After 18 months on combination immunotherapy, scans showed no trace of cancer. He’s been in remission for over four years.Why Some Tools Are Still Too Risky
Not every new gadget is ready for prime time. DermaSensor, for example, increases the number of biopsies by 30% because it’s too sensitive. That’s not just inconvenient-it’s expensive and stressful. A biopsy isn’t harmless. It leaves scars. It causes anxiety. And if you’re getting biopsies for harmless moles, you’re not helping-you’re harming. The same goes for AI tools that don’t explain their decisions. If a doctor can’t understand why the system flagged a spot, they won’t trust it. That’s why explainable AI is non-negotiable now. The iToBoS scanner wins here. It doesn’t just say “cancer.” It shows the color gradient, the border irregularity, the asymmetry-exactly what a dermatologist looks for. That builds trust. There’s also the issue of integration. Most clinics still use old electronic health records. New AI tools don’t always plug in. One dermatology practice in Ohio spent six months trying to connect their AI system to their EMR. They gave up. The software vendor didn’t support it. That’s a huge barrier. Even the best tech fails if it doesn’t fit into daily workflow.
What You Can Do Right Now
You don’t need a high-tech scanner to save your life. Here’s what actually works:- Check your skin monthly. Use a mirror. Look for moles that are asymmetrical, have uneven borders, vary in color, are larger than a pencil eraser, or are changing over time.
- Don’t ignore moles on your scalp, between toes, under nails, or on your buttocks. Melanoma hides in plain sight.
- If you have a family history of melanoma or more than 50 moles, see a dermatologist every year.
- Wear sunscreen daily. Not just at the beach. UV damage adds up-even on cloudy days.
- Know your risk. Fair skin, sunburns as a kid, tanning bed use-these raise your chances.
What’s Next for Melanoma Care
The future isn’t just better tools-it’s smarter ones. Imagine a system that combines your skin scan, your blood test for genetic markers, your sun exposure history, and your immune profile-all in one risk score. That’s what researchers are building. Some are even testing AI that can predict which patients will respond to which immunotherapy, based on their tumor’s DNA. The goal? Personalized prevention. Instead of screening everyone the same way, we’ll know who needs monthly checks, who needs a scanner, and who just needs to stay out of the sun. The data is clear: early detection saves lives. Immunotherapy turns deadly cancer into a manageable condition. The pieces are here. Now, we just need to make them accessible-to every skin tone, every income level, every corner of the world.Can melanoma be cured if caught early?
Yes. When melanoma is found before it spreads beyond the top layer of skin, the 5-year survival rate is over 99%. Surgery to remove the lesion is usually all that’s needed. Early detection is the most effective treatment.
Is immunotherapy better than chemotherapy for melanoma?
For advanced melanoma, immunotherapy is now the first-line treatment because it’s more effective and has fewer side effects than chemotherapy. Chemo rarely works on melanoma. Immunotherapy trains your immune system to attack cancer cells, leading to longer survival and, in some cases, complete remission.
Do AI skin scanners replace dermatologists?
No. AI tools assist doctors-they don’t replace them. Even the best AI has false positives and struggles with rare cases or darker skin tones. A dermatologist combines AI results with clinical experience, patient history, and physical exam to make the final call.
How accurate are AI tools for melanoma detection?
The most advanced AI systems, like SegFusion and DenseNet-201, achieve 94-96% accuracy on standardized skin images. But real-world accuracy drops to 85-90% due to lighting, skin tone, and image quality. Accuracy also depends on the tool-DermaSensor has high sensitivity but low specificity, meaning it catches most melanomas but flags too many benign moles.
Are home skin scanners worth buying?
Most consumer-grade apps and handheld devices aren’t FDA-cleared or clinically validated. They may give false reassurance or cause unnecessary panic. Stick to proven methods: monthly self-checks and annual dermatologist visits. If you’re high-risk, ask your doctor about FDA-approved tools like DermaSensor that are used in clinical settings.
Can melanoma come back after immunotherapy?
Yes. While many patients achieve long-term remission, melanoma can return. Some tumors develop resistance to immunotherapy drugs. That’s why ongoing monitoring with scans and blood tests is critical-even after treatment ends. Researchers are now testing combination therapies and vaccines to prevent recurrence.








10 Comments
Francine Phillips
December 3, 2025 AT 06:26Wow this is wild I just stared at my mole for 10 minutes and now I’m convinced it’s cancer
parth pandya
December 3, 2025 AT 10:05did u know dermasensor is only 26% specifity?? that means like 3 outta 4 people get biopsied for nothin 😭 i had one last year and it was just a pimple with a tan
Makenzie Keely
December 3, 2025 AT 11:12Let me just say this: early detection isn’t just a slogan-it’s a lifeline. I had a mole on my scalp that I ignored for two years because it ‘didn’t look like the pictures.’ When I finally went in, it was stage 2. Surgery, no chemo, no immunotherapy. Just a scalpel and a prayer. Now I check my skin every Sunday morning with a hand mirror and a cup of coffee. It takes five minutes. Five minutes could save your life. And yes, I know it’s annoying to check between your toes-but trust me, melanoma doesn’t care how awkward you feel. Also: sunscreen daily. Even when it’s cloudy. Even when you’re inside. UV rays don’t take days off. And if you’re dark-skinned? Don’t let anyone tell you you’re ‘immune.’ I’ve seen melanoma under fingernails on Black patients. It’s rare, but it happens. And it’s deadly when missed. So check. Your. Skin. Every. Month. And if you’re high-risk? See a derm. Not a dermatology app. A real doctor. With real training. And yes, I’m yelling. Because lives are on the line.
Joykrishna Banerjee
December 3, 2025 AT 17:54How quaint. You're all celebrating AI like it's the Second Coming-but let’s be honest: these algorithms are trained on datasets that are 90% Caucasian skin. The iToBoS scanner? Beautiful engineering. But when it flags a seborrheic keratosis on a Fitzpatrick V patient as ‘suspicious,’ and then the dermatologist-trained in the same biased system-agrees, you’re not saving lives. You’re perpetuating healthcare apartheid. And don’t even get me started on ‘explainable AI’-it’s just lipstick on a pig if the underlying data is rotten. We need decolonized datasets, not more ‘innovation’ that caters to the privileged. 🤷♂️
Gavin Boyne
December 4, 2025 AT 04:46So we’ve got AI that can detect melanoma with 99% accuracy… but only if you’re white, rich, and live near a university hospital. Meanwhile, my cousin in rural Mississippi still uses a magnifying glass and Google Images. The real breakthrough isn’t the tech-it’s the fact that we still haven’t fixed access. We’re designing Ferrari engines for horses. And yes, I’m being sarcastic. But also… not. 😏
Charles Moore
December 5, 2025 AT 21:08Just wanted to say thank you to everyone who’s pushing for better tools and more inclusive research. I’m a nurse in a rural clinic, and we don’t have a dermoscope, let alone an AI scanner. But we do have monthly skin checks with patients during their annual visits. We use a ruler for the ABCDE rule, we ask about family history, and we never say ‘it’s probably fine.’ Sometimes, the most powerful tool is just paying attention-and listening. Keep pushing for equity, but don’t forget the power of the human touch. We’re not replacing doctors-we’re helping them do their jobs better.
Albert Essel
December 6, 2025 AT 22:36One thing I’ve learned from working in oncology: immunotherapy isn’t magic. It’s biology. And biology is messy. Some patients go into complete remission. Others don’t respond at all. And some respond… then relapse. That’s why ongoing monitoring is non-negotiable. I’ve seen patients celebrate year one, then get hit with recurrence at year three. The science is incredible-but so is the emotional toll. We need better biomarkers to predict who will respond. And we need to stop treating immunotherapy like a cure-all. It’s a tool. A powerful one. But not a panacea.
Myson Jones
December 8, 2025 AT 01:32Just wanted to add a quick note: if you're reading this and you're a primary care provider-please, please, please don’t dismiss a patient’s concern just because ‘it doesn’t look like melanoma.’ I’ve had patients come in with lesions under their nails, on their palms, even on their genitals. One woman had a dark streak on her thumbnail. She thought it was a bruise. It was melanoma. Early. We caught it. She’s fine now. Don’t wait for textbook cases. Listen. Examine. Refer. It’s not complicated. And it saves lives.
Ignacio Pacheco
December 8, 2025 AT 05:35So the wearable patch that detects electricity changes in moles… sounds like sci-fi. But I’m skeptical. Ten people? That’s not a study, that’s a pilot. And ‘statistically significant’ doesn’t mean ‘clinically useful.’ Also-how do you wear it for 24 hours without it falling off? Sweat? Shower? What if you’re hairy? This feels like a Kickstarter campaign with a lab coat.
Jim Schultz
December 9, 2025 AT 07:18Oh wow, another ‘melanoma is scary’ post. Congrats, you’ve read a medical article. But let’s be real-99% survival rate? That’s because you’re not counting the people who died from unnecessary biopsies. You’re not counting the anxiety, the cost, the scars. You’re not counting the fact that 70% of melanomas appear on people who never tanned. So what’s the point? Stop fear-mongering. Stop buying gadgets. Just live your life. And if you’re really worried? Go to the doctor. Not the internet. Not the app. The actual human with the stethoscope. And for god’s sake, stop using sunscreen like it’s armor. You’re not a vampire. You’re a person. Go outside. Be healthy. Stop obsessing.