Every time you pick up a prescription, there’s a small sticker on the bottle. Maybe it’s red. Maybe it says take with food. Or do not crush. You might glance at it, shrug, and toss the bottle in your bag. But those stickers aren’t just paperwork-they’re your last line of defense against serious harm. In fact, nearly half of all preventable medication errors in the U.S. happen because patients don’t understand what these labels actually mean.
What Those Stickers Are Really For
Those little stickers aren’t optional. They’re legally required by the FDA. Every prescription container must carry warnings that prevent injury. These aren’t suggestions. They’re safety rules built on real data-cases where people ended up in the ER because they took a pill with grapefruit juice, or drove after a new painkiller made them drowsy, or crushed a capsule thinking it’d work faster. The most serious warnings are called Black Box Warnings. You’ll find them printed in bold, boxed text on the drug’s official prescribing guide. About 40% of new drugs approved between 2013 and 2017 had one. These aren’t warnings about mild side effects. They’re for risks that can cause death or permanent damage-like heart failure, liver failure, or suicidal thoughts. If your pill has this, you need to know why it’s there.Color Matters More Than You Think
Not all stickers are created equal. Color isn’t just for decoration. Studies show patients instinctively read color as a danger signal. Red means stop. Yellow means be careful. Blue or green? Most people think those are just reminders, not warnings. A 2017 study found that 85% of people correctly understood a red label saying do not operate machinery. But only 45% got the meaning of a blue one saying the same thing. That’s a huge gap. If your pharmacist puts a blue sticker on a sedative, you might ignore it. And that’s exactly what happens-people end up behind the wheel, dizzy and disoriented, because they didn’t treat the warning seriously.What Common Warnings Actually Mean
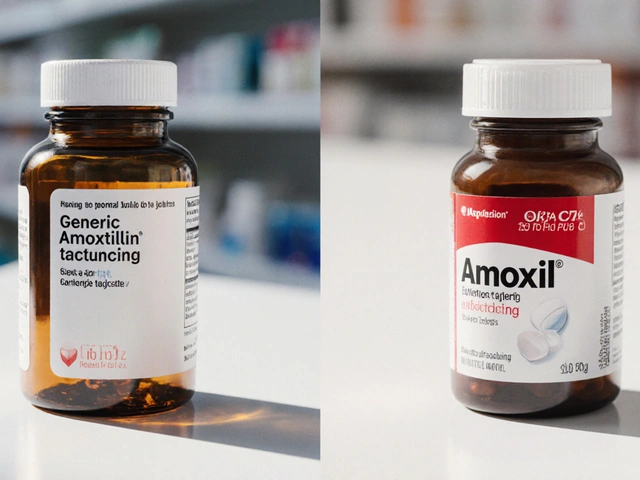
Let’s break down the most confusing ones:- Take on empty stomach - Means at least one hour before or two hours after eating. Food can block absorption. Some antibiotics, like amoxicillin, become useless if taken with milk or yogurt.
- Take with food - Not a suggestion. It’s to protect your stomach. Drugs like ibuprofen or certain antidepressants cause nausea or ulcers if taken on an empty stomach. Eating doesn’t make them work better-it keeps you from getting sick.
- Do not crush or chew - Many pills are designed to release slowly. Crush them, and you get a full dose all at once. That’s how overdoses happen. One patient crushed a long-acting opioid and died within 20 minutes.
- Refrigerate - This isn’t about freshness. Some medicines break down at room temperature. Insulin, certain antibiotics, and even some cancer drugs can lose potency if left out. The right temperature is 2-8°C (36-46°F). A warm car or kitchen counter can ruin them.
- Avoid alcohol - It’s not just about getting drunk. Alcohol can make painkillers toxic to your liver, boost drowsiness from anxiety meds, or cause dangerous blood pressure drops with heart meds.
- Avoid sunlight - Some drugs make your skin ultra-sensitive. Tetracycline, for example, can cause severe burns from normal sun exposure. You might think you’re just being cautious, but this isn’t about tanning-it’s about avoiding blistering.

Why You’re Probably Misreading Them
The FDA admits most warning labels are written for doctors, not patients. The average American reads at a 7th-grade level. But many labels are written at a 12th-grade level or higher. Words like contraindicated, adverse reaction, or hepatic impairment are meaningless to most people. Even simple phrases trip people up. A study found that 91% of patients misunderstood for external use only. Some thought it meant use on your skin (correct). Others thought it meant don’t swallow it (also correct). But 27% thought it meant don’t use it at all-and stopped taking their medicine. That’s not confusion. That’s a health crisis. Symbols make it worse. A little icon of a hand with a line through it? Some people think it means radioactive. Others think it means take with shaking. One patient saw the do not crush symbol and thought it meant crush it to make it work faster. He ended up in the hospital.What Works Better
The good news? We know how to fix this. In pilot programs at Kaiser Permanente, they replaced complex labels with plain language and pictures. Instead of do not operate heavy machinery, they wrote do not drive. Instead of take on empty stomach, they wrote take 1 hour before breakfast. Results? Comprehension jumped from 55% to 89%. That’s not magic. That’s clarity. Some pharmacies now use QR codes. Scan it, and a short video explains the warning in simple terms. Mayo Clinic tested this with 500 patients. Comprehension rose by over 50%. It’s not science fiction-it’s happening now.
How to Protect Yourself
You don’t have to wait for the system to change. Here’s what to do every time you get a new prescription:- Check the pill. Does the shape, color, and imprint match what the label says? If not, ask. Counterfeit pills are a growing problem.
- Read the color. Red? That’s serious. Yellow? Be cautious. Blue or green? Still read it. Don’t assume it’s low priority.
- Ask the pharmacist to explain. Say: “Can you tell me what this warning means in plain words?” Don’t be shy. They’re trained for this.
- Use the teach-back method. After they explain, repeat it back in your own words. “So if I take this with grapefruit, my blood pressure could drop too low?” If they nod, you got it right.
- Keep the Patient Prescribing Information sheet. Yes, it’s long. But it has the full details. Don’t throw it away. Store it with your meds.
Why This Isn’t Just Your Problem
Medication errors cause 1.3 million injuries and 7,000 deaths every year in the U.S. That’s more than car crashes. Most of these are preventable. And it’s not just about you. If you misunderstand a warning and end up in the ER, it affects your family, your insurance, your coworkers, your hospital system. The FDA is finally moving toward simpler labels. By 2026, 20 high-risk drugs will have standardized, easy-to-read warnings. But until then, you’re the last line of defense.What to Do If You’re Still Confused
If you’re unsure about a warning, don’t guess. Don’t Google it and hope for the best. Call your pharmacist. They’re the experts on your meds. Most will answer for free, even if you didn’t fill the script there. If you’re on multiple drugs, ask for a medication review. Many pharmacies offer this at no cost. They’ll check for dangerous interactions you didn’t know about. And if you ever feel like a warning doesn’t make sense? Speak up. You’re not being difficult. You’re being smart.What does a black box warning mean on a prescription label?
A black box warning is the strongest safety alert the FDA requires. It means the drug has been linked to serious, potentially life-threatening side effects-like organ failure, severe allergic reactions, or increased risk of suicide. It doesn’t mean you can’t take the drug, but you and your doctor need to weigh the risks carefully. These warnings appear on the official prescribing information and are sometimes repeated on the pharmacy label if the risk is high enough.
Why do some pills say "take with food" and others say "take on an empty stomach"?
It depends on how the drug is absorbed. Some medications need food to reduce stomach upset or to help your body absorb them properly. Others are blocked by food-like certain antibiotics or thyroid meds. If food interferes, the drug won’t work. If food protects your stomach, skipping it could cause nausea or ulcers. Always follow the exact instruction. It’s not a suggestion-it’s science.
Can I ignore a warning if I’ve taken the medicine before without problems?
No. Your body changes. So do your other medications. A warning you ignored last time might be dangerous now. For example, if you started a new blood pressure drug, grapefruit juice that was fine before could now cause your pressure to drop dangerously low. Or if you’ve gained weight or developed kidney issues, your body may process the drug differently. Always treat every warning as new.
What should I do if I accidentally break a warning?
Don’t panic, but don’t wait. Call your pharmacist or doctor right away. Tell them exactly what happened-what you took, when, and what the warning said. They’ll tell you if you need to be checked. For example, if you crushed a slow-release pill, they might ask you to monitor for dizziness or rapid heartbeat. If you took a drug with alcohol, they might check your liver function. Acting fast can prevent a hospital visit.
Are color-coded warning stickers standardized across all pharmacies?
No. There’s no national standard for sticker colors. Red usually means danger, but it’s not required. Some pharmacies use red, yellow, and green. Others use only white with bold text. That’s why you can’t rely on color alone. Always read the words. If a warning is important, it will be written out clearly-even if the color is inconsistent.