When you’re older, your body doesn’t process medicine the same way it did when you were 30. That’s not just a myth-it’s science. A 75-year-old taking the same dose of a blood pressure pill as a 50-year-old might end up with dangerously low blood pressure, dizziness, or even a fall. This isn’t about being weak or fragile. It’s about how aging changes your liver, kidneys, fat, and muscle-and how those changes affect every pill you swallow.
Why Older Bodies Need Different Doses
Your body’s ability to handle medicine changes in four key ways as you age. First, your stomach produces less acid, which means some drugs don’t get absorbed as well. Second, your body gains fat and loses muscle. That means drugs that stick to fat-like certain antidepressants or painkillers-can build up in your system longer than expected. Third, your liver slows down. By age 70, many people process drugs 30% to 50% slower than they did at 40. And fourth, your kidneys filter blood less efficiently. After age 30, kidney function drops about 8 mL per minute every decade. By 70, many people have less than half the kidney clearance they had in their 20s.This isn’t theoretical. A 2022 study in JAMA Internal Medicine found that 35% of hospital admissions for people over 65 were caused by bad reactions to medications. Many of those reactions happened because the dose was never adjusted for age.
The ‘Start Low, Go Slow’ Rule
Doctors have a simple rule for older adults: start low, go slow. It’s been around since the 1980s, backed by decades of research from the American Geriatrics Society and the FDA. That means if a medication normally starts at 10 mg for an adult, the starting dose for someone over 65 might be 2.5 mg or 5 mg. Then, the dose is slowly increased-over weeks, not days-while watching for side effects.Take gabapentin, a common nerve pain drug. The standard starting dose is 300 mg once a day. For an older adult, especially with reduced kidney function, that dose is often cut in half-to 100 mg or 150 mg. Even then, it’s increased only if needed and tolerated.
Metformin, used for type 2 diabetes, is another example. In younger people, it’s safe at higher doses. But for seniors, it’s stopped entirely if kidney function drops below 30 mL/min. Between 30 and 45, the dose is cut by half. Why? Because metformin builds up in the blood if kidneys can’t clear it, and that can cause a rare but deadly condition called lactic acidosis.
How Doctors Calculate the Right Dose
There’s no one-size-fits-all formula, but doctors use a few trusted tools. The most common one is the Cockcroft-Gault equation. It estimates how well your kidneys are working based on your age, weight, and a simple blood test for creatinine. The formula looks like this:CrCl = [(140 - age) × weight (kg)] / [72 × serum creatinine (mg/dL)]
For women, you multiply the result by 0.85. If your result is below 50 mL/min, most drugs cleared by the kidneys need a dose reduction. For example, digoxin (used for heart rhythm) has a target blood level of 0.5-0.9 ng/mL in seniors-much lower than the 0.8-2.0 ng/mL range for younger adults. Too high, and you risk dangerous heart rhythms.
For drugs processed by the liver, doctors use the Child-Pugh score. It looks at liver function through blood tests and physical signs like fluid buildup in the belly. A score of 7-9 means moderate liver damage-doses need to be cut by half. A score of 10-15 means severe damage-many drugs should be avoided entirely.

High-Risk Medications for Seniors
Some medications are just too dangerous for older adults, no matter the dose. The 2023 Beers Criteria® from the American Geriatrics Society lists 30 classes of drugs that should be avoided or used with extreme caution. These include:- Benzodiazepines (like diazepam or lorazepam)-increase fall risk by 50%
- NSAIDs (like ibuprofen or naproxen)-triple the risk of stomach bleeding
- Anticholinergics (like diphenhydramine or oxybutynin)-double dementia risk with long-term use
- Antipsychotics (used off-label for dementia behavior)-increase stroke and death risk
- Warfarin-requires 20-30% lower doses in seniors due to slower metabolism and higher bleeding risk
Many of these drugs are still prescribed because they’re familiar or easy to write. But they’re not safe. A 2020 study in Annals of Internal Medicine found that 40% of nursing home residents were on at least one Beers Criteria drug. That’s not normal-it’s a warning sign.
The Problem with Polypharmacy
The average American over 65 takes five prescription drugs. One in four takes ten or more. This is called polypharmacy-and it’s the biggest risk factor for bad drug reactions. Each new pill adds a chance for interaction. A blood thinner plus a painkiller plus a diuretic plus a statin? That’s four different ways your body can get overwhelmed.Dr. Dima Mazen Qato’s 2016 study showed that 55% of seniors take five or more meds. And the more you take, the harder it is to know which one is causing a problem. Did you feel dizzy because of your blood pressure pill? Or the sleeping pill? Or the combination? Without careful review, it’s guesswork.
This is why the Medication Appropriateness Index (MAI) exists. It’s a 10-point checklist doctors can use to rate each drug: Is it appropriate? Is the dose right? Is it needed? A score above 18 means your medication list needs a serious overhaul.
What Works in Real Life
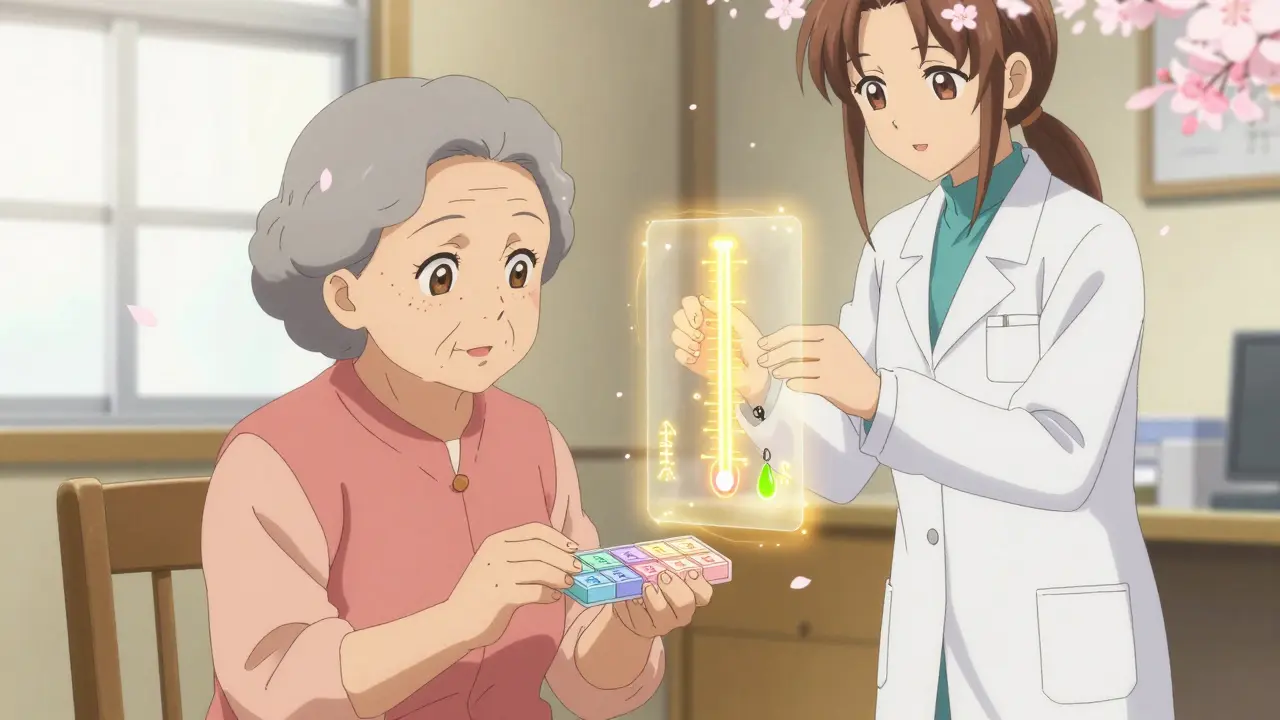
The best ideas don’t just live in textbooks-they work in clinics. One of the most successful programs is the Pharm400 model from the University of North Carolina. Pharmacists meet with seniors weekly, sort their pills into daily blister packs, check kidney and liver function, and adjust doses based on how they’re feeling. In a 2021 study, this approach cut hospital visits by 22% in just one year.Another simple trick? The “brown bag review.” Ask patients to bring every pill, supplement, and over-the-counter medicine they take to their appointment. More than half of seniors don’t know what’s in their own medicine cabinet. One study found that 37% of seniors were taking something their doctor didn’t know about-often herbal supplements or leftover antibiotics.
Electronic health records can help too. Alerts that pop up when a doctor prescribes a kidney-cleared drug to someone with low creatinine clearance reduce errors by 53%. But only 65% of clinics use them consistently.

The Gaps in the System
Here’s the uncomfortable truth: most drugs weren’t tested on people over 75. A 2019 FDA analysis of 218 major clinical trials found that 40% of participants were under 65. That means doctors are guessing how drugs work in older adults. For 70% of medications commonly used in seniors, there’s little to no data on safe dosing.And even when data exists, many doctors aren’t trained to use it. A 2021 AMA survey found that 65% of U.S. physicians felt unprepared to adjust doses for aging bodies. That’s why pharmacists are becoming essential. Their training focuses on drug interactions, metabolism, and dosing. Studies show pharmacist-led reviews reduce medication errors by 67%.
What’s Changing Now
The field is shifting. The FDA now requires age-stratified data in all new drug trials. The Beers Criteria® now includes frailty measures-not just age. And AI tools like MedAware are being tested to predict dangerous dosing combinations before they happen. In a 2023 Johns Hopkins pilot, the AI cut dosing errors by 47%.Future guidelines will likely move away from age-based dosing and toward functional age. If you walk slowly, get tired easily, or forget to take pills, your body may be aging faster than your birth certificate says. Tests like the Timed Up and Go (timing how long it takes to stand, walk 3 meters, turn, and sit back down) are now used to guide dosing. If your time is over 12 seconds, you’re considered frail-and your meds need a closer look.
The goal by 2030? Personalized dosing based on your liver, kidneys, and how your body actually responds-not just your age. That’s not science fiction. It’s the next step in safe care.
What You Can Do
If you or a loved one is over 65 and taking multiple medications:- Ask your doctor: “Is this dose right for my age and kidney function?”
- Request a creatinine blood test if you haven’t had one in the last year.
- Bring all your pills to every appointment-even the ones you haven’t taken in months.
- Ask if any meds can be stopped or lowered.
- Know the names of your drugs and why you take them.
- Watch for dizziness, confusion, falls, or sudden fatigue-these are red flags.
Medication isn’t harmless just because a doctor wrote it. In older adults, every pill carries risk. The right dose can mean better health. The wrong one can mean a hospital bed.
Why can’t older adults take the same medication doses as younger people?
Because aging changes how the body absorbs, distributes, metabolizes, and removes drugs. Kidney and liver function decline, body fat increases, and muscle mass decreases. These changes mean drugs stay in the system longer and can build up to toxic levels-even at standard doses.
What is the Cockcroft-Gault equation used for?
It estimates kidney function (creatinine clearance) using age, weight, and blood creatinine levels. Doctors use it to decide whether to lower the dose of drugs cleared by the kidneys, like antibiotics, painkillers, or diabetes meds.
Which medications are most dangerous for seniors?
According to the 2023 Beers Criteria®, high-risk drugs include benzodiazepines (increase fall risk), NSAIDs (cause stomach bleeding), anticholinergics (linked to dementia), and antipsychotics (raise stroke risk). Even common OTC sleep aids like diphenhydramine fall into this category.
How do I know if my medication dose is too high?
Watch for new symptoms after starting or changing a drug: dizziness, confusion, falls, extreme fatigue, nausea, or memory lapses. These are often signs of overdose in older adults. Don’t wait for a doctor’s visit-call your provider if you notice these.
Can pharmacists help with medication adjustments?
Yes. Pharmacists specialize in drug interactions, metabolism, and dosing. Studies show pharmacist-led reviews reduce medication errors by 67% in seniors. Ask your doctor if you can be referred to a geriatric pharmacist for a full medication review.
What is a brown bag review?
It’s when you bring all your medications-prescription, over-the-counter, vitamins, and supplements-to a doctor’s appointment. This helps catch duplicates, expired drugs, or interactions your doctor doesn’t know about. It’s one of the most effective ways to prevent harmful medication errors.






10 Comments
Aaron Bales
January 1, 2026 AT 09:18My dad’s on six meds. Last year he fell after a new blood pressure script. Turned out the dose was for a 40-year-old. We pushed back, got it cut in half, and he’s been stable since. Start low, go slow isn’t just advice-it’s survival.
Doctors forget aging isn’t a number. It’s a system.
Lawver Stanton
January 2, 2026 AT 13:53Okay, but let’s be real-this whole ‘aging body’ thing is just Big Pharma’s way of selling more tests, more labs, more ‘specialist consultations.’ You think they really care if your kidneys are working? Nah. They care if your insurance covers the $300 creatinine panel and the $120 pharmacist consult.
I’ve seen grandmas get their meds reviewed by a pharmacist who barely looked at their list. Meanwhile, the doc’s still prescribing benzos like they’re cough drops. This isn’t science-it’s a revenue stream dressed up in jargon.
And don’t get me started on ‘functional age.’ What’s next? ‘Functional wealth’? ‘Functional dignity’? We’re turning medicine into a personality quiz.
Meanwhile, my 82-year-old neighbor still takes ibuprofen like candy. He’s sharp, walks 3 miles a day, and doesn’t fall. So why is his dose being cut? Because the algorithm says so. Not because he’s broken.
It’s all just fear-mongering with a side of bureaucracy.
Sara Stinnett
January 3, 2026 AT 22:15How delightfully patronizing. We’re told to ‘start low, go slow’-as if older adults are children who can’t handle responsibility. The real tragedy isn’t the dosage-it’s the infantilization. We’ve turned geriatric care into a moral fable where the elderly are fragile vessels needing constant correction.
And yet, the same system that demands we ‘respect autonomy’ in youth insists we surrender it the moment we hit 65. ‘You’re too old to know what’s best for you’-said by a 32-year-old resident who’s never met a patient over 70.
The Beers Criteria? A checklist for cultural anxiety, not clinical wisdom. Who decided that ‘increased dementia risk’ is a valid reason to deny a person relief from incontinence? That’s not medicine. That’s eugenics with a stethoscope.
And let’s not pretend the ‘brown bag review’ is a solution. It’s a Band-Aid on a hemorrhage. The system doesn’t want to fix dosing-it wants to make you feel guilty for taking pills.
My grandmother took three benzos a day for 18 years. She lived to 94. Sharp as a tack. Walked daily. Loved jazz. The doctors called her ‘high-risk.’ I call her a miracle.
Maybe the problem isn’t the pills. Maybe it’s the presumption that aging equals decay.
linda permata sari
January 4, 2026 AT 21:10In Indonesia, we don’t have fancy equations or AI tools. Our grandparents take what the village doctor says-often half a pill, sometimes crushed in honey. No blood tests. No charts. Just observation.
My auntie, 83, takes a quarter of her metformin because she gets dizzy. She doesn’t know what ‘CrCl’ means. But she knows her body. And she’s been walking to market every morning for 60 years.
Maybe the answer isn’t more data. Maybe it’s more trust.
Also, we call it ‘medicine of the elders’-not ‘geriatric dosing.’ It’s not a category. It’s a relationship.
Brandon Boyd
January 6, 2026 AT 13:17Big win for awareness here! This is exactly the kind of info that saves lives-and it’s not talked about enough.
One thing I tell my senior clients: your meds aren’t ‘set and forget.’ They’re living things. Your body changes, your meds need to change too.
Ask your pharmacist to do a med sync. It’s free at most pharmacies. They’ll sort your pills, flag interactions, and tell you what’s actually still needed.
And if your doctor brushes you off? Find a new one. Your health isn’t negotiable.
You’ve got this. One pill at a time.
Branden Temew
January 7, 2026 AT 05:26So we’re supposed to believe that a 70-year-old’s liver is a broken toaster and a 25-year-old’s is a Ferrari? Cute.
Meanwhile, the same people who say ‘start low, go slow’ are the ones prescribing 100mg of gabapentin to a 72-year-old with a creatinine of 1.2… then blaming the patient for ‘non-compliance’ when they’re too dizzy to stand.
Here’s the real problem: medicine treats aging like a disease to be managed, not a stage of life to be understood.
And yet, we’ll spend $200K on a hip replacement but won’t pay a pharmacist $50 to review your meds.
Charming.
Frank SSS
January 9, 2026 AT 03:28Yeah, I read all this. And I’m just… tired.
My mom’s on 11 meds. She forgets half of them. The rest she takes at weird times because the bottles look alike. The doctor says ‘start low, go slow’-but never says how slow. Or low.
I spent three hours last week trying to figure out if her dizziness was from the blood pressure pill or the sleeping pill or the antidepressant she’s been on since 2008.
And now you want me to bring a brown bag? I’m not a pharmacist. I’m her son. I work 60 hours a week. I don’t have time to decode this mess.
So yeah. The system’s broken. But I’m not the one who broke it. And I’m not the one who can fix it.
Just… let me sleep.
Paul Huppert
January 10, 2026 AT 06:59This is really helpful. I’ve been trying to explain to my mom why she shouldn’t take OTC sleep aids anymore, but I didn’t know about the Beers Criteria. I’ll print this out and take it to her next appointment.
Also, the brown bag idea is genius. I never thought to ask her to bring everything-she just says ‘I don’t take anything weird.’ Turns out, she’s been taking melatonin, turmeric, and three different heartburn pills from the pharmacy.
Thanks for making this so clear.
Hanna Spittel
January 10, 2026 AT 12:20They’re lying. 🤫
They don’t want you to know that 90% of these ‘dose adjustments’ are just to push you into Medicare Advantage plans. More meds = more data = more $$$ for the insurance bots.
And the ‘AI tools’? They’re trained on data from people who died. So they’re basically predicting your death and adjusting your pills to match.
Bring your brown bag. Then burn it. 🕯️
Brady K.
January 10, 2026 AT 15:53Let’s reframe this: aging isn’t a pharmacokinetic problem-it’s a systems failure. We’ve outsourced care to algorithms while abandoning human judgment.
The Cockcroft-Gault equation? A 1970s approximation. The Beers Criteria? A 2023 checklist written by committee. The Pharm400 model? A pilot that works because someone actually *listened*.
But here’s the real jargon: ‘medication appropriateness.’ What does that even mean? Appropriate for whom? The insurer? The EMR? The patient?
They call it ‘personalized medicine.’ But it’s just standardized fear wrapped in a white coat.
Meanwhile, my 81-year-old uncle takes 12 pills. He’s still fishing every Saturday. His creatinine is 1.4. His kidneys? Fine. His spirit? Unbroken.
Maybe the real metric isn’t clearance rates.
Maybe it’s whether you still get up to watch the sunrise.
Just saying.