When you take carbamazepine for epilepsy or nerve pain, you’re not just taking a pill-you’re managing a complex chemical dance inside your body. Even small changes in the brand or manufacturer of your generic carbamazepine can throw that balance off. And for many patients, the consequences aren’t theoretical-they’re seizures, dizziness, rashes, or worse.
Why carbamazepine is different from other generics
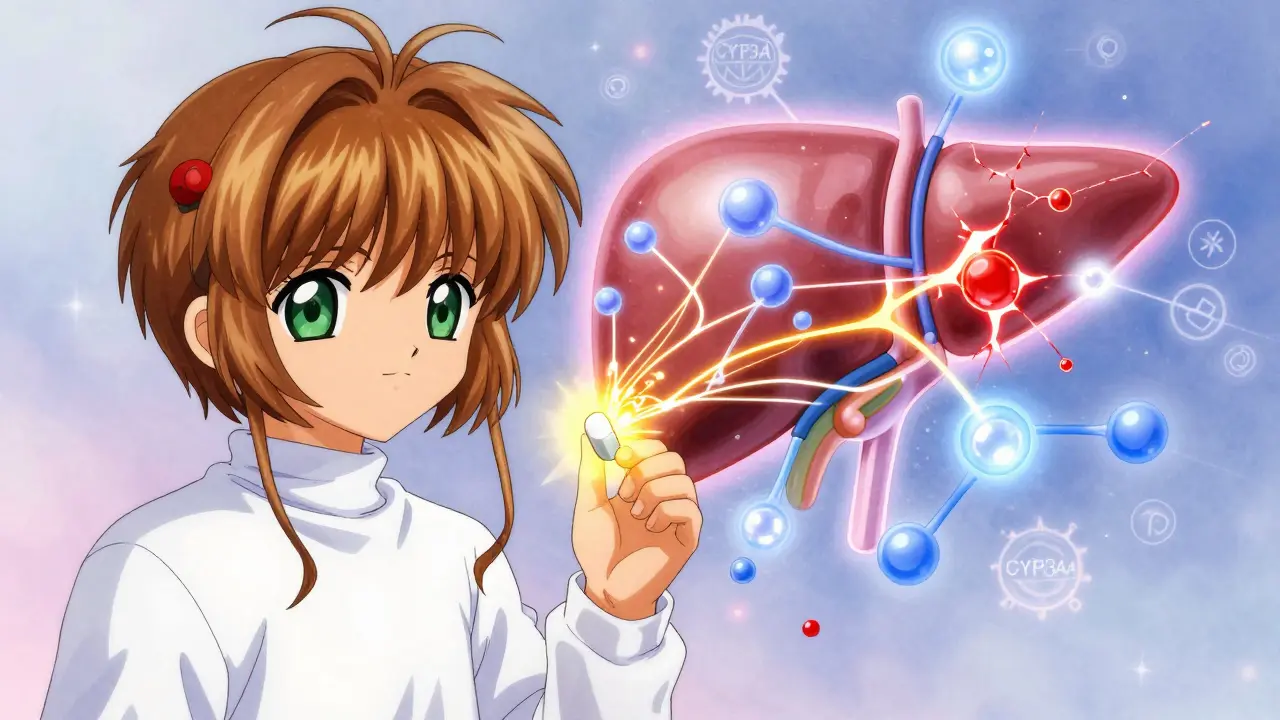
Most drugs have a wide safety margin. Take ibuprofen: if your dose is a little high or low, you might feel a bit more or less pain relief, but you won’t end up in the hospital. Carbamazepine? Not even close. Its therapeutic range is razor-thin: 4 to 12 mcg/mL in the blood. Go below 4, and seizures might return. Rise above 12, and you risk drowsiness, double vision, or even life-threatening toxicity. The problem isn’t just the narrow range-it’s how the drug behaves. Carbamazepine is a potent enzyme inducer. That means it doesn’t just get metabolized by your liver-it actively speeds up the liver’s ability to break down other drugs. This effect starts within 48 hours of starting the medication and peaks in 2 to 3 weeks. It doesn’t stop when you stop taking it, either. The enzyme boost lingers for 1 to 2 weeks after discontinuation. This autoinduction means carbamazepine essentially turns your liver into a drug-processing factory that’s always running at full speed. And because it induces CYP3A4-the most important enzyme in drug metabolism-it affects roughly half of all medications you might be taking. That includes blood thinners like warfarin, heart drugs like amlodipine, immunosuppressants like cyclosporine, and even HIV medications. If you’re on any of these, your doctor needs to know you’re taking carbamazepine. Otherwise, you could end up with a failed transplant, a stroke, or an untreated infection.Generic versions aren’t all the same
There are 32 approved generic versions of immediate-release carbamazepine tablets and 18 of extended-release formulations in the U.S. alone. On paper, they’re all bioequivalent. That means, in healthy volunteers, their absorption and peak concentration are within 80-125% of the brand-name drug. But here’s the catch: those studies are done on 24 to 36 healthy people, not on someone with epilepsy, kidney disease, or 5 other medications. A 2018 study in Epilepsia followed 327 patients who were switched between different generic carbamazepine products. Over 12% had a drop in seizure control or new side effects. Nearly 8% ended up in the emergency room. Why? Because even tiny differences in how the tablet breaks down in the stomach-differences that meet FDA standards-can cause big changes in people whose bodies are already sensitive. Extended-release versions like Tegretol XR, Carbatrol, or Equetro are especially tricky. They’re designed to release the drug slowly over time. But if one generic uses slightly larger beads or a different coating, the release pattern can change. One patient in a 2023 study reported that switching from one generic to another caused her carbamazepine levels to drop from 7.2 to 4.8 mcg/mL-right out of the therapeutic range-even though her dose didn’t change. She went from 1-2 seizures a month to 4-5 a week.
Gender, genetics, and hidden risks
Men and women metabolize carbamazepine differently. Women tend to break it down faster because of higher CYP3A4 activity. That means women, especially those of childbearing age, often need higher doses to stay in range. A 2021 study in JAMA Neurology found women switching between generics had 22% more breakthrough seizures than men. Hormones play a role too-estrogen can further speed up metabolism, which is why some women have more seizures during certain parts of their cycle. Then there’s genetics. If you carry the HLA-B*1502 gene variant-common in people of Asian descent-you’re at 10 times higher risk of developing Stevens-Johnson Syndrome (SJS), a deadly skin reaction. The FDA recommends genetic testing before starting carbamazepine for anyone with ancestry from Southeast Asia. If you’re positive for this gene, carbamazepine should be avoided entirely. Alternatives like levetiracetam are safer. Even more surprising: researchers have now identified 17 genetic variations that affect how your body handles carbamazepine. One of them, CYP3A4*22, means you need 25% less of the drug to reach the same blood level. Without knowing your genes, you’re dosing blind.
What you should do if you’re on carbamazepine
If you’re taking carbamazepine, here’s what matters:- Stick with the same manufacturer. If your pharmacy switches your generic, ask for the brand name or the exact generic you’ve been on. Many neurologists now write “dispense as written” (DAW code 1) on prescriptions to block automatic substitution.
- Get your blood tested. Therapeutic drug monitoring isn’t optional-it’s essential. Check your levels before any switch, again 7-14 days after, and then at 4 weeks. If your level changes by more than 15%, your dose needs adjustment.
- Know your interactions. Tell every doctor, pharmacist, and even your dentist you’re on carbamazepine. Common culprits: birth control pills (can fail), statins (can cause muscle damage), and antibiotics like erythromycin (which can spike carbamazepine levels).
- Watch for signs of trouble. New dizziness, rash, nausea, confusion, or more seizures? Don’t wait. Call your neurologist immediately. These aren’t just side effects-they could be early warning signs of toxicity or loss of seizure control.






13 Comments
Ariel Edmisten
February 7, 2026 AT 20:31Just stuck with the same generic. No switching. My neurologist wrote DAW-1 and I’ve been fine for 3 years. Don’t mess with it.
Sarah B
February 8, 2026 AT 16:47Pharmacies switch generics to save pennies and patients pay with seizures
Heather Burrows
February 8, 2026 AT 21:43It’s funny how we treat medicine like it’s just a commodity. Like a box of cereal. But this isn’t about cost-it’s about the quiet, invisible collapse of someone’s nervous system. We don’t see it until it’s too late.
Savannah Edwards
February 9, 2026 AT 07:53I’ve been on carbamazepine for 11 years. I switched generics once-just once-because my insurance forced it. That week, I was dizzy 24/7, couldn’t focus at work, and had two tiny tremors I’d never felt before. I called my neurologist immediately. She said, "You’re lucky you noticed. Most people don’t until they’re in the ER." Now I pay out of pocket for the same brand. Worth every penny. Also, I’m a woman in my 30s and I’ve had to bump my dose up 3 times since starting because my hormones shift with my cycle. They don’t tell you that part. Ever.
Gouris Patnaik
February 9, 2026 AT 09:45India has better generic standards than the US. We test on real patients, not college kids. You think your FDA is strict? It’s a joke. My cousin took a US generic and had a rash. Here, they’d never approve it without 6 months of real-world data.
Lakisha Sarbah
February 11, 2026 AT 08:13so i got my levels checked after switching and they dropped 20%… my doc was like "oh yeah that happens" and just upped my dose. no one warned me. why is this not standard?
Amit Jain
February 12, 2026 AT 00:34THIS IS WHY AMERICA IS BROKE. Pharmacies care about profit. Patients get seizures. Doctors are asleep. And the FDA? They’re still testing on 24 healthy people in 2024. Wake up. This isn’t a bug. It’s a feature of capitalism.
Eric Knobelspiesse
February 13, 2026 AT 13:10wait so if you have the hla-b*1502 gene and take carbamazepine you get like 90% chance of skin peeling off? that’s wild. i had no idea. my aunt had sjs and we thought it was just "bad luck"
Mayank Dobhal
February 15, 2026 AT 03:11My brother took carbamazepine after a car accident. Switched generics. Two weeks later: seizures. ER. ICU. Now he’s on brand. I swear to god, if you’re on this med, don’t let your pharmacy touch it. Call them. Threaten them. Do whatever it takes.
Jesse Lord
February 16, 2026 AT 14:37Hey everyone, if you’re on this med and you’re scared, you’re not alone. I’ve been there. Talk to your neurologist. Get tested. Ask for a copy of your blood levels. You deserve to know what’s happening in your body. And if your pharmacist tries to switch you? Say no. Politely. Firmly. You’ve got a right to stability.
AMIT JINDAL
February 17, 2026 AT 22:49Let’s be real. The whole system is rigged. Big Pharma makes the brand. Then they let generics compete on price. But carbamazepine? It’s not like Advil. It’s a precision instrument. And we’re letting pharmacists play Russian roulette with people’s brains. And the FDA? They’re too busy approving new weight-loss drugs to care. 😔
Catherine Wybourne
February 19, 2026 AT 19:08Interesting how we treat epilepsy like it’s just a medical issue, not a social one. People lose jobs. Lose insurance. Lose dignity because their pharmacy switched a pill. We talk about innovation in medicine, but we won’t fix this? I’m from the UK-we have a national monitoring system. No one gets switched without consent. It’s not that hard. It’s just not a priority.
Ashley Hutchins
February 21, 2026 AT 00:37why do people even take generics if they know this? if you’re too cheap to pay for the brand then maybe you shouldn’t be on a drug that can kill you