When you start taking an SGLT2 inhibitor for type 2 diabetes, you might not expect to feel dizzy or unusually thirsty. But these side effects aren’t rare-they’re built into how the drug works. SGLT2 inhibitors like empagliflozin, dapagliflozin, and canagliflozin aren’t just sugar-lowering pills. They act like mild diuretics, pulling excess glucose and salt out of your body through urine. That’s great for your heart and kidneys. But it also means your body loses water-and that’s where problems can start.
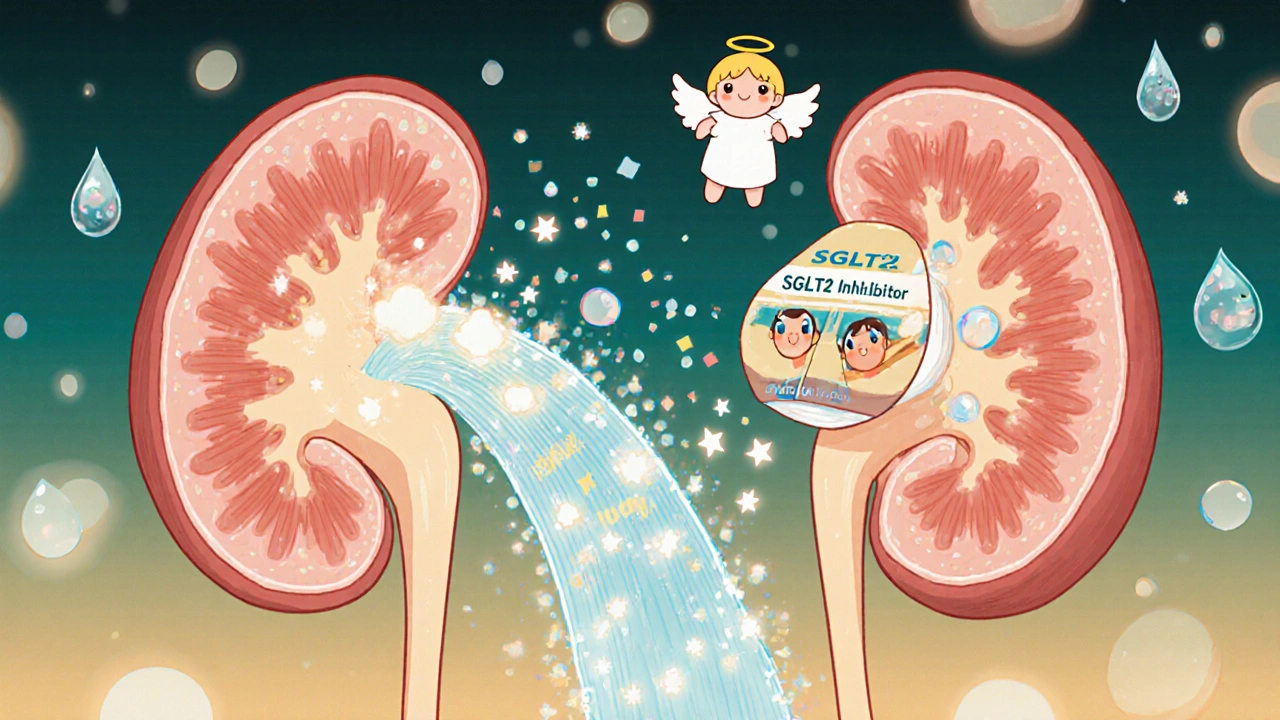
How SGLT2 Inhibitors Work Like Diuretics
Your kidneys normally reabsorb almost all the glucose filtered from your blood. SGLT2 proteins in the proximal tubules are responsible for this. When you take a drug like empagliflozin (a sodium-glucose cotransporter-2 inhibitor used to treat type 2 diabetes and heart failure), it blocks those proteins. Glucose that would’ve been saved now gets flushed out-about 70 to 100 grams per day. That’s roughly 250 to 400 calories lost daily, just through urine.
But here’s the catch: glucose doesn’t leave alone. It drags sodium and water with it. This isn’t just sugar loss-it’s fluid loss. You’re losing 1 to 1.5 liters of fluid in the first week. That’s like skipping a full day’s water intake. The result? A natural, drug-induced diuresis. It’s why these drugs lower blood pressure and reduce heart failure hospitalizations. But it’s also why some people feel lightheaded or dry-mouthed.
Why Dehydration Happens-and Who’s at Risk
Dehydration from SGLT2 inhibitors isn’t a myth. In clinical trials, 1.3% to 2.8% of users reported volume depletion symptoms, compared to under 1% on placebo. That might sound low, but it adds up fast in real life. The risk jumps significantly if you’re over 65, have kidney issues (eGFR below 60), or are already on other diuretics like furosemide.
Older adults are especially vulnerable. Their bodies don’t trigger thirst as strongly, so they don’t drink enough to replace what’s lost. A 72-year-old on canagliflozin (an SGLT2 inhibitor with higher diuretic potential than other drugs in its class) might not feel thirsty even after sweating at the grocery store or walking the dog. By the time they feel dizzy, they’re already dehydrated.
Other risk factors include:
- Starting the drug while on ACE inhibitors or ARBs
- Low baseline blood pressure (below 120 mmHg systolic)
- Illnesses like vomiting, diarrhea, or fever
- Hot weather or intense exercise without extra fluids
One study found that patients with systolic blood pressure under 120 mmHg had over three times the risk of symptomatic low blood pressure. If you’re already on meds to lower your pressure, adding an SGLT2 inhibitor can push you over the edge.
Dizziness: More Than Just a Nuisance
Dizziness is the most common symptom tied to this fluid shift. In trials, 3.5% to 5.8% of people taking SGLT2 inhibitors reported dizziness-compared to 2.5% to 3.2% on placebo. That’s about 1 in 20 people. It usually shows up in the first 2 to 4 weeks, right when your body is adjusting to losing fluid.
Most of the time, it’s orthostatic-meaning it happens when you stand up. Your blood pressure drops suddenly because your volume is low. Your brain doesn’t get enough blood for a second, and you feel like you’re going to pass out. In 63% of cases, dizziness is directly linked to orthostatic hypotension: a systolic drop of 20 mmHg or more when standing.
Who’s most likely to get it?
- People over 75 (risk doubled)
- Those taking diuretics (risk over three times higher)
- Anyone with systolic blood pressure below 130 mmHg
Canagliflozin has the highest reported rate of dizziness among SGLT2 inhibitors-6.3 cases per 1,000 patient-years. Dapagliflozin and empagliflozin are slightly lower. But even the "safer" ones can cause trouble if you’re in a high-risk group.
Real-world stories back this up. On Reddit, one user wrote: "Started Jardiance last week. Got dizzy standing up. My doctor said it’s normal for the first month." Another said: "Canagliflozin made me so dehydrated I had to stop after 3 weeks-constant thirst, dry mouth, no relief."
How Blood Pressure Drops-And Why That’s Actually Good
Here’s the twist: the same mechanism that causes dizziness also protects your heart. SGLT2 inhibitors lower systolic blood pressure by 4 to 6 mmHg on average. Diastolic drops by 1 to 2 mmHg. That might seem small, but it’s enough to reduce stroke risk and slow kidney damage.
How? Two ways:
- Preload reduction: Less fluid in your blood vessels means your heart doesn’t have to work as hard to pump.
- Afterload reduction: Your arteries become more flexible, reducing resistance. Studies show arterial stiffness drops by 8-12% over 24 weeks.
This is why SGLT2 inhibitors are now recommended for heart failure-even in people without diabetes. The DAPA-HF (a landmark clinical trial showing dapagliflozin reduced cardiovascular death in heart failure patients) trial found a 17% drop in cardiovascular death. The EMPEROR-Reduced (a major trial proving empagliflozin improves outcomes in heart failure with reduced ejection fraction) trial showed similar results.
These drugs don’t just lower sugar. They change how your body handles fluid, pressure, and stress on your heart and kidneys. The trade-off? A little dizziness for a lot of protection.
What Doctors Do to Keep You Safe
Good prescribers don’t just hand you a script and hope for the best. They take steps to reduce risk:
- Start with a lower dose-e.g., 10 mg of empagliflozin instead of 25 mg
- Check your blood pressure and heart rate before starting
- Ask about your fluid intake, kidney function, and other meds
- Schedule a follow-up in 7 to 10 days to check for dizziness or weight loss
- Measure orthostatic blood pressure: sitting, then standing
If your systolic pressure drops below 90 mmHg when standing-or you feel faint-your doctor may pause the drug temporarily. They might also reduce your loop diuretic dose by 25-50% instead of stopping the SGLT2 inhibitor entirely. Why? Because the long-term benefits often outweigh the short-term side effects.
Most endocrinologists now recommend increasing fluid intake by 500 to 1,000 mL per day when starting these drugs. That’s about 2 to 4 extra cups of water. Don’t wait until you’re thirsty. Drink regularly, especially in heat or after exercise.
What You Can Do to Stay Safe
You’re not powerless here. You can manage these side effects yourself:
- Drink water consistently. Aim for at least 8 cups a day. More if it’s hot or you’re active.
- Stand up slowly. Give your body time to adjust. Hold onto furniture if you feel wobbly.
- Watch your weight. A sudden drop of more than 2 kg (4.4 lbs) in a week could mean too much fluid loss.
- Don’t skip meals. Low blood sugar can worsen dizziness.
- Hold the drug during illness. If you’re vomiting, have diarrhea, or have a fever, pause your SGLT2 inhibitor until you’re back to normal.
- Report dizziness early. Don’t wait until you fall. Tell your doctor-it’s fixable.
Many people report dizziness fades after 2 to 4 weeks as their body adapts. But if it doesn’t, or if you feel faint often, don’t ignore it. Your doctor can adjust your dose or timing.
The Bigger Picture: Benefits vs. Side Effects
Yes, SGLT2 inhibitors can make you dizzy and dehydrated. But they also cut your risk of heart failure hospitalization by up to 30%. They slow kidney disease progression by 30-50%. They reduce the chance of dying from heart-related causes by nearly 20%.
Dr. Bertram Pitt, lead researcher on the DAPA-HF trial, put it simply: "Six lives saved per 100 patients treated over 18 months. That’s worth a little dizziness."
For most people with type 2 diabetes-especially those with heart or kidney disease-the benefits far outweigh the risks. But for others-older adults, those with low blood pressure, or people on multiple diuretics-the risks need careful management.
This isn’t a drug for everyone. But for the right person, it’s life-changing. The key isn’t avoiding side effects entirely-it’s recognizing them early and acting on them before they become dangerous.
Do SGLT2 inhibitors cause dehydration?
Yes. SGLT2 inhibitors cause fluid loss by making your kidneys excrete glucose and sodium, which pulls water with them. This leads to mild diuresis. About 1.3% to 2.8% of users experience volume depletion symptoms like dry mouth, dizziness, or low blood pressure. Risk is higher in older adults, those with kidney disease, or people on other diuretics.
Why do SGLT2 inhibitors cause dizziness?
Dizziness usually happens because of orthostatic hypotension-your blood pressure drops when you stand up. This is caused by reduced fluid volume from increased urination. The effect is strongest in the first few weeks of treatment. About 63% of dizziness cases are linked to this drop in blood pressure upon standing.
Do SGLT2 inhibitors lower blood pressure?
Yes. On average, they lower systolic blood pressure by 4-6 mmHg and diastolic by 1-2 mmHg within 1-2 weeks. This happens because of fluid loss and improved artery flexibility. The effect is independent of blood sugar control and benefits people with or without diabetes.
Who should avoid SGLT2 inhibitors?
People with very low blood pressure (systolic under 110 mmHg), severe kidney impairment (eGFR below 30), or those already on high-dose diuretics should use caution. Elderly patients over 75, especially with multiple medications, need close monitoring. These drugs are not recommended if you’re dehydrated or have a history of frequent volume depletion.
Can I still take SGLT2 inhibitors if I get dizzy?
Often, yes. Dizziness usually improves after a few weeks. Your doctor may lower your dose, advise more fluids, or reduce other blood pressure meds. Stopping the drug isn’t always necessary-especially if you have heart or kidney disease. The cardiovascular benefits often outweigh the temporary side effects.
How long does it take for SGLT2 side effects to go away?
Most side effects like dizziness and increased urination peak in the first 2-4 weeks and then improve as your body adjusts. Weight loss from fluid loss usually stabilizes after 1-2 weeks. If symptoms persist beyond 4 weeks or worsen, talk to your doctor-your dose may need adjustment.
Is it safe to drink alcohol while taking SGLT2 inhibitors?
Alcohol can increase dehydration and lower blood pressure further, making dizziness worse. It’s best to limit alcohol, especially when you first start the medication. If you drink, do so in moderation and always drink water alongside it.
What Comes Next?
If you’re on an SGLT2 inhibitor and feel fine, keep going. These drugs are changing how we treat diabetes, heart failure, and kidney disease. But if you’re feeling dizzy, thirsty, or lightheaded, don’t brush it off. Talk to your doctor. A simple adjustment-more water, a lower dose, or pausing another medication-can make all the difference.
These drugs aren’t magic. They’re powerful tools with real trade-offs. The goal isn’t to avoid side effects completely-it’s to use them wisely. With the right monitoring and habits, you can get the benefits without the risks.






10 Comments
Peter Aultman
November 15, 2025 AT 09:23Started Jardiance last month and yeah the dizziness hit hard the first week
Stood up from the couch and saw stars
Dr told me to drink more water and stand slow
Now I carry a bottle everywhere and it’s fine
Worth it for the heart stuff
Barry Sanders
November 15, 2025 AT 15:58Typical pharma marketing. They sell you a drug that makes you dehydrated and call it a ‘cardioprotective benefit’.
Stop pretending this is medicine. It’s a diuretic with a fancy name.
And now they want you to drink more water? That’s not treatment, that’s damage control.
Jane Johnson
November 17, 2025 AT 09:09While I appreciate the clinical data presented, I must point out that the normalization of iatrogenic volume depletion as an acceptable trade-off reflects a troubling trend in modern endocrinology.
The emphasis on HbA1c reduction and cardiovascular endpoints often obscures the lived experience of patients who are left lightheaded, fatigued, and anxious about standing up.
There is an ethical dimension to prescribing medications that induce physiological stress as a mechanism of action.
Perhaps we should reconsider whether the marginal gains justify the daily discomfort.
Sean Hwang
November 17, 2025 AT 10:57Man I was scared when I started canagliflozin
Kept getting dizzy walking to the bathroom
My doc said drink a glass of water every time you pee
Did that for a week and now I dont even think about it
Also lost 5lbs in 10 days but not fat lol
My blood pressure dropped from 135 to 122
Worth it if you got heart issues
Sean Evans
November 17, 2025 AT 20:19LOL so now we’re supposed to be grateful for being dehydrated? 🤡
These drugs are basically making your kidneys throw sugar in the toilet while you pay $500 a month for it.
And don’t even get me started on the ketoacidosis risk-y’all act like it’s a myth.
My cousin ended up in the ER with DKA because she ‘didn’t feel thirsty’.
Stop glorifying side effects. This is not wellness. It’s chemical roulette.
🩸💧💀
Brittany C
November 18, 2025 AT 12:48As a nephrology nurse practitioner, I’ve seen the flip side of this: patients on SGLT2i with eGFR 45 and on furosemide 80mg daily who present with orthostatic hypotension and acute kidney injury.
The guidelines say ‘monitor’, but in practice, the follow-up window is often too wide.
Baseline orthostatic vitals are non-negotiable.
And yes, the cardiovascular benefits are real-but they require intentional, not passive, management.
Don’t let the hype override clinical caution.
kshitij pandey
November 20, 2025 AT 04:25Bro I’m from India and we don’t have much access to these drugs
But I read this and I’m like wow
My uncle had diabetes and heart problem
He was on diuretics and felt weak all day
But if he could take this and feel better later
Then maybe it’s worth trying
Just drink water and take it slow
Life is long, health is everything
Scarlett Walker
November 20, 2025 AT 11:16I started on dapagliflozin and thought I was dying
Thirsty all the time, dizzy, felt like I was going to pass out
But then I started drinking water like it was my job
And now I feel better than I have in years
My A1c dropped from 8.9 to 6.7
And I’m not on insulin anymore
It’s not magic, it’s just science with a side of hydration
Don’t panic, just adapt
Anjan Patel
November 21, 2025 AT 08:25Y’all are missing the point
This isn’t about dehydration
This is about the medical system turning patients into lab rats
They push these drugs because they’re profitable
Not because they’re safe
And then they blame you when you get dizzy
‘Just drink more water!’
Like that fixes the problem
It doesn’t
It just makes you feel guilty for being sick
Chris Ashley
November 21, 2025 AT 22:05My mom’s on empagliflozin and she’s 78
She was so dizzy she couldn’t walk to the mailbox
Doc lowered her dose and told her to sit on the edge of the bed for 30 sec before standing
Now she’s fine
She says she feels lighter
Like her heart isn’t working so hard
She’s not going back
Just gotta adjust