Every year, hundreds of thousands of people in the U.S. are harmed because of mistakes made when doctors write prescriptions. These aren’t rare accidents. They’re preventable. And as a patient, you have more power to stop them than you might think.
What Happens When a Prescription Goes Wrong
A prescription error isn’t just a typo. It’s a medical mistake that can lead to hospitalization, long-term damage, or even death. The most common errors? Wrong dose, wrong drug, or unclear instructions. A doctor might write ‘5.0 mg’ thinking it’s clear, but if the zero is smudged, the pharmacist reads it as ‘50 mg’-ten times too much. Or they might use ‘U’ for units, which looks like a ‘0’-leading to a fatal insulin overdose. These aren’t hypotheticals. Between 2010 and 2020, the FDA documented 128 deaths from just two types of decimal errors: missing leading zeros (like .5 mg read as 5 mg) and trailing zeros (like 10.0 mg read as 100 mg).
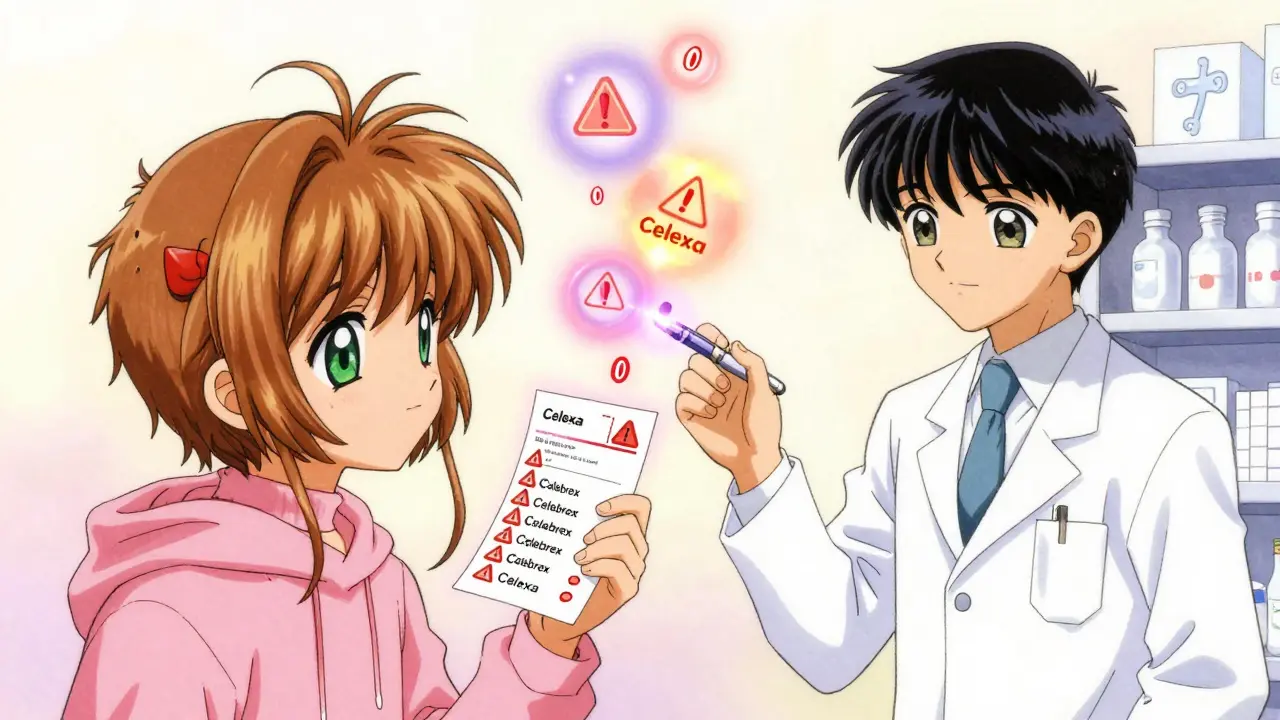
Drug names can be just as dangerous. ‘Celebrex’ and ‘Celexa’ sound alike but do completely different things-one treats arthritis, the other depression. Mixing them up can have serious consequences. The same goes for ‘Zyprexa’ and ‘Zyrtec,’ or ‘HC’ for hydrocortisone mistaken for heparin, a blood thinner. These aren’t rare mix-ups. They happen every day.
The Hidden Costs of a Bad Prescription
These errors don’t just hurt patients-they cost the system billions. Medication errors add $42 billion to U.S. healthcare costs each year. That’s 5% of total spending. Pharmacists spend nearly 19 minutes per prescription just double-checking what the doctor wrote. In 2015, that number was just over 6 minutes. Why the jump? Because prescriber errors have gotten worse, not better. Even with electronic systems, doctors still make mistakes. A 2019 study found that 34% of new error types came from e-prescribing systems themselves, like accidentally selecting ‘50 mg’ instead of ‘5 mg’ because the numbers are too close on a dropdown menu.
Time pressure is a big reason why. Physicians in busy clinics average just 17 seconds per prescription. When you’re rushing, you’re more likely to skip details, use shortcuts, or miss critical info like kidney function or drug interactions. One study found that 68% of primary care doctors make at least one prescribing error every month. Internists average 2.3 errors per month. That’s not negligence-it’s a broken system.
How to Spot a Problem Before It’s Too Late
You don’t need to be a doctor to catch a dangerous prescription. You just need to know what to look for. Here’s a simple checklist based on FDA and patient safety guidelines:
- Full drug name-No abbreviations. ‘Lamictal’ should be written as ‘lamotrigine.’ Abbreviations like ‘MS’ for morphine sulfate can be confused with ‘MgSO4’ (magnesium sulfate), which is deadly if given to the wrong patient.
- Precise dosage-Look for leading zeros (0.5 mg, not .5 mg) and no trailing zeros (5 mg, not 5.0 mg). These small formatting choices prevent tenfold dosing errors.
- Clear instructions-Avoid ‘QD’ (daily), ‘BID’ (twice daily), or ‘TID’ (three times daily). These abbreviations are outdated and dangerous. The instructions should say ‘once daily,’ ‘twice daily,’ etc.
- Correct quantity-If you’re prescribed 30 pills for a 7-day course, that’s a red flag. Ask why. Is it a refill error? A typo?
- Why you’re taking it-The prescription should include the reason, like ‘for high blood pressure’ or ‘for migraine.’ If it’s blank, ask.
- Doctor’s contact info-If the phone number or clinic name is missing, that’s a red flag. Legitimate prescriptions always include this.
- Expiration date-Prescriptions expire. If it’s not there, ask when it’s no longer valid.
A 2022 University of Michigan study found that patients who used this checklist caught 63% of prescription errors before even reaching the pharmacy. Patients who didn’t use it caught only 22%.

High-Risk Medications You Need to Watch For
Not all drugs are created equal when it comes to danger. The most lethal errors involve what’s called ‘high-alert medications.’ These include:
- Insulin
- Warfarin (a blood thinner)
- Opioids like oxycodone
- IV heparin
- Chemotherapy drugs
These make up only 8% of all prescriptions, but they cause 72% of fatal errors. If you’re taking one of these, double-check everything. Use the ISMP’s ‘error-prone drug pairs’ list to compare your medication with look-alike names. For example, ‘Lamictal’ (used for seizures) is often confused with ‘Lamivudine’ (an HIV drug). The wrong one could be deadly.
Ask the Right Questions
Don’t be afraid to speak up. The ‘Ask Me 3’ program-used by hospitals across the U.S.-teaches patients to ask three simple questions:
- What is my main problem?
- What do I need to do?
- Why is it important for me to do this?
A 2021 study in JAMA Network Open found that patients who asked these questions reduced their risk of medication errors by 44%. When you ask why, you’re not being difficult-you’re protecting your life.
Another powerful tool is the ‘teach-back method.’ After the doctor or pharmacist explains how to take your medicine, repeat it back in your own words. ‘So I take one pill every morning with food, right?’ If they correct you, you’ve caught a mistake. Johns Hopkins found this method reduces misunderstandings by 81%.
What to Do When You Get Your Prescription
When you pick up your meds at the pharmacy, don’t just take the bottle and leave. Compare the label to your checklist. Does the drug name match? Is the dose the same? Is the reason listed? If anything looks off, ask the pharmacist to double-check with the prescriber. Pharmacies now spend nearly 20 minutes per script verifying prescriptions-much of it fixing errors that came from the doctor’s office. They’re trained to catch mistakes. Use them.
If you get an electronic prescription, ask for a printed copy to review before leaving the clinic. Many patients assume e-prescriptions are foolproof. They’re not. A 2023 study showed that 31% of doctors bypass safety alerts in their electronic systems because they’re annoying. That means a warning that says ‘This drug interacts with your heart medication’ might never pop up.

Technology Can Help-But Only If You Use It
Apps like MedSafety let you take a photo of your prescription and scan it for errors. In a 2023 pilot study, these tools caught 68% more errors than patients checking manually. They flag things like missing leading zeros, confusing abbreviations, or dangerous drug combinations.
By 2025, federal rules will require all electronic health records to send you real-time updates about your prescriptions via secure text or patient portals. This means you’ll get a message like: ‘Your new prescription is lamotrigine 100 mg once daily for seizures.’ If that’s not what your doctor told you, you’ll know right away.
And by 2030, experts predict 90% of prescriptions will require you to confirm the details before the pharmacy fills them. Imagine a pop-up on your phone: ‘Confirm: You’re getting insulin 10 units daily for diabetes. Is this correct?’ If you say yes, it goes through. If not, the doctor gets notified. This isn’t science fiction-it’s coming.
What If You Can’t Read or Understand the Prescription?
One in three adults in the U.S. has low health literacy. That means they struggle to understand medical terms, instructions, or forms. If this sounds like you or someone you care for, you’re not alone. And you’re not powerless.
Many communities now have ‘Script Check’ volunteers-trained advocates who help older adults and people with limited literacy review prescriptions for free. In its first year, this program in 37 states caught over 8,200 dangerous errors. Ask your local hospital, library, or senior center if they offer this service.
You can also bring someone with you to appointments-a family member, friend, or caregiver. Two sets of eyes are better than one. And if you’re unsure, always ask for a written copy you can take home and study.
Why This Matters More Than Ever
Prescription errors are the most preventable type of medical mistake. Yet, since 2000, we’ve only reduced them by 15%. That’s not progress. It’s a failure. But change is happening. More patients are learning how to speak up. More pharmacies are checking twice. More doctors are being held accountable.
You’re not just a passive receiver of care. You’re the last line of defense. The system won’t fix itself. But you can help fix it-one prescription, one question, one ‘no, that doesn’t look right’ at a time.
What are the most common prescription errors?
The most common errors include wrong dosage (especially decimal mistakes like .5 mg read as 5 mg), incorrect drug names (like mixing up Celebrex and Celexa), unclear instructions (using abbreviations like QD or U for units), and failure to check for drug interactions. These account for over 80% of all prescription-related errors.
Can I really catch a mistake before the pharmacy fills it?
Yes. A 2022 study showed patients who checked their prescriptions using a simple seven-point checklist caught 63% of errors before reaching the pharmacy. That’s more than double the rate of those who didn’t check. Always compare the written prescription to what your doctor told you.
Why do doctors make so many errors?
Time pressure is the biggest factor. Doctors in busy clinics spend an average of just 17 seconds per prescription. Workload, poor training in prescribing, and outdated habits like using dangerous abbreviations all contribute. Even electronic systems can cause errors if doctors skip safety alerts or pick the wrong option from a dropdown menu.
What should I do if I think my prescription is wrong?
Don’t take it to the pharmacy yet. Call your doctor’s office and ask them to verify the prescription. If you’re unsure, ask the pharmacist to contact the prescriber. It’s better to delay the fill than risk taking the wrong medication. Pharmacies are trained to catch errors and will gladly help you confirm.
Are electronic prescriptions safer than handwritten ones?
Electronic prescriptions reduce handwriting errors by over 50%, but they introduce new risks. Studies show 34% of new error types come from e-prescribing systems-like selecting the wrong dose from a dropdown menu or ignoring safety alerts. The key is not just using technology, but using it correctly and staying vigilant.
How can I help a family member catch prescription errors?
Bring them to appointments, help them check the prescription using the seven-point checklist, and use the teach-back method: ask them to explain how to take the medicine in their own words. If they have low health literacy, look for local ‘Script Check’ programs that offer free help reviewing prescriptions.