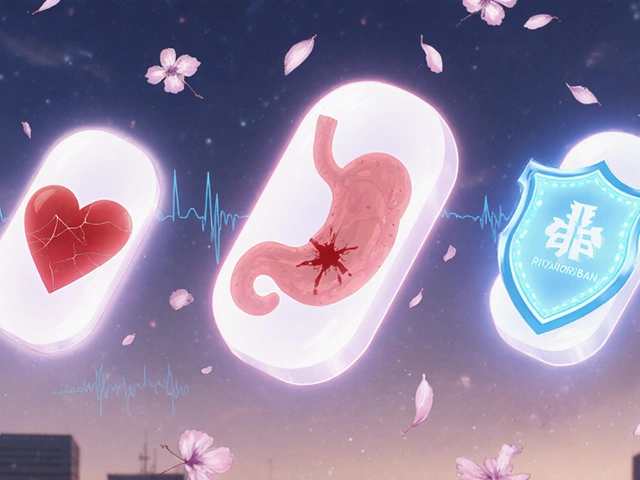
When a senior falls, the fear isn’t just about a bruise or a sprain. It’s about anticoagulants - the very drugs meant to prevent life-threatening strokes - turning a simple tumble into a medical emergency. Many families and even some doctors assume that if an older person is prone to falls, they shouldn’t take blood thinners. But the science tells a different story. For seniors with atrial fibrillation, skipping anticoagulants because of fall risk often means trading a small chance of injury for a much higher chance of death or disability from stroke.
Why Seniors Need Anticoagulants
Atrial fibrillation, or AFib, is an irregular heartbeat that affects nearly 9 out of every 100 adults over 65. In AFib, the heart doesn’t pump blood properly, letting clots form in the left atrium. If a clot breaks loose, it can travel to the brain and cause a stroke. The older you are, the higher the risk. At age 80-89, the chance of having a stroke from AFib jumps to 23.5% per year. That’s more than one in four people. Anticoagulants cut that risk in half or more. Warfarin, used since the 1950s, reduces stroke risk by about 65%. Newer drugs - called DOACs (direct oral anticoagulants) like apixaban, rivaroxaban, dabigatran, and edoxaban - work just as well, and often better. Apixaban, for example, reduced stroke and systemic embolism by 21% compared to warfarin in patients over 75. And here’s the kicker: these drugs lower the risk of bleeding in the brain by 34% compared to warfarin. That’s critical because brain bleeds are the most dangerous kind.The Fall Risk Myth
It’s understandable to worry. If someone has fallen twice in the past year, it’s natural to think: “Don’t give them blood thinners - they could bleed out from a simple slip.” But multiple large studies have shown that the fear of falls is overblown when it comes to stopping anticoagulants. The BAFTA trial, which studied patients with an average age of 81.5, found that those on anticoagulants had a 52% lower risk of stroke or systemic embolism than those on aspirin. And there was no significant increase in major bleeding. The ARISTOTLE trial showed that even in patients over 85, apixaban still reduced stroke risk without increasing fatal bleeds. In fact, the oldest patients - those 90 and older - got the most net benefit from anticoagulation. Why? Because their stroke risk was so high, and their bleeding risk, while real, didn’t outweigh the protection. A 2023 review in the Journal of Hospital Medicine called stopping anticoagulants due to fall risk “inappropriate practice.” The American College of Cardiology, American Heart Association, and Heart Rhythm Society all agree: age and a history of falls are not reasons to withhold anticoagulation. The real danger isn’t falling - it’s not treating the AFib.
How DOACs Compare to Warfarin
Warfarin works, but it’s messy. It needs frequent blood tests (INR checks every 4 weeks on average) to make sure the dose is right. Too little, and strokes happen. Too much, and bleeding risks spike. In real life, many elderly patients spend less than 65% of their time in the safe range - meaning they’re either under- or over-protected most of the time. DOACs changed the game. They don’t need regular blood tests. Dosing is fixed: one or two pills a day. Apixaban 5mg twice daily, rivaroxaban 20mg once daily, dabigatran 150mg twice daily - all proven safe and effective in seniors. They’re also easier on the kidneys than warfarin in some cases, though kidney function still matters. Here’s how they stack up:| Drug | Dose | Stroke Risk Reduction | Major Bleeding Risk vs. Warfarin | Renal Clearance | Reversal Agent |
|---|---|---|---|---|---|
| Warfarin | Adjustable (INR 2-3) | ~65% | Reference | Minimal | Vitamin K, PCC |
| Apixaban (Eliquis) | 5mg twice daily | 21% better than warfarin | 31% lower | 27% | Andexanet alfa |
| Rivaroxaban (Xarelto) | 20mg once daily | Non-inferior to warfarin | Similar | 33% | Andexanet alfa |
| Dabigatran (Pradaxa) | 150mg twice daily | 88% vs. placebo | 20% lower | 80% | Idarucizumab |
| Edoxaban (Savaysa) | 60mg once daily | Comparable to warfarin | 8.5% absolute reduction | 50% | Andexanet alfa |
Apixaban stands out for seniors. In the ARISTOTLE trial, patients over 75 had fewer major bleeds on apixaban than on warfarin. It’s also the only DOAC with strong data in patients over 90. For someone with mild kidney decline - common in older adults - apixaban is often the safest choice.
When Falls Are a Real Concern
That doesn’t mean fall risk should be ignored. A fall on anticoagulants can be deadly. Data from Minnesota hospitals shows that 90% of fall-related deaths in seniors involve either people over 85 or those on anticoagulants. But here’s the key: it’s not the anticoagulant alone that’s the problem. It’s the combination of multiple risks - poor balance, weak bones, dim lighting, loose rugs, or other medications like benzodiazepines that make you dizzy. The solution isn’t to stop the blood thinner. It’s to reduce the chance of falling. Studies show that a simple, three-part plan cuts falls by up to 35%:- Exercise: The Otago Exercise Program - a home-based balance and strength routine - reduces falls by a third in seniors.
- Medication review: Cut or lower doses of sleep aids, painkillers, or antidepressants that cause dizziness.
- Home safety: Install grab bars, remove throw rugs, add nightlights, and fix uneven steps.
Doctors should use tools like the HAS-BLED score, which includes fall history as one factor - but it’s not a stop sign. A score of 3 or higher means you need to monitor more closely, not stop treatment.
Why So Many Seniors Are Still Left Untreated
Despite the evidence, only about half of eligible seniors with AFib get anticoagulants. Among those 85 and older, it drops to 48%. Why? Because doctors are afraid. A 2021 survey found that 68% of primary care doctors would withhold anticoagulation from an 85-year-old with two falls - even if their stroke risk score (CHA₂DS₂-VASc) was 4, which means they have a 7% annual risk of stroke. That’s a huge gap between guidelines and practice. Families are scared too. On Reddit, caregivers share stories of doctors refusing to prescribe blood thinners because “they fall too much.” One mother wrote: “They said, ‘We can’t give him Eliquis - he fell last month.’ I cried. I knew he needed it.” The truth? These patients are more likely to have a stroke than to die from a fall. A 2023 analysis found that for every 100 octogenarians treated with anticoagulants for a year, 24 strokes are prevented - and only 3 major bleeds occur. That’s a net gain of 21 lives spared or disabilities avoided.What to Do Next
If you or a loved one has AFib and is over 65, here’s what to ask:- What’s my CHA₂DS₂-VASc score? (If it’s 2 or higher, anticoagulation is recommended.)
- What’s my kidney function? (Creatinine clearance matters for DOAC dosing.)
- Can we start with apixaban? (It’s the safest DOAC for seniors.)
- What’s the plan to reduce fall risk? (Exercise, home safety, medication review.)
- What happens if I fall? (Know the reversal agents - andexanet alfa works for apixaban and rivaroxaban.)
Don’t let fear of falling keep you from preventing a stroke. The data is clear: for seniors with AFib, anticoagulants save more lives than they endanger - if you manage the risks smartly.
Should I stop my blood thinner if I fall once?
No. A single fall is not a reason to stop anticoagulation. The risk of stroke from untreated atrial fibrillation is far greater than the risk of bleeding from a fall. Instead, focus on identifying why the fall happened - was it dizziness, poor lighting, or a medication side effect? Fix those causes, not the anticoagulant.
Are DOACs safer than warfarin for seniors?
Yes, for most seniors. DOACs like apixaban and rivaroxaban have lower risks of brain bleeds and don’t require frequent blood tests. Apixaban, in particular, has shown better safety in patients over 75 and is often preferred for older adults. Warfarin is still used, especially if kidney function is very low or cost is a barrier, but DOACs are now the first-line choice for most.
Can I take aspirin instead of a blood thinner?
No. Aspirin reduces stroke risk by only about 22%, while anticoagulants reduce it by 60-70%. For atrial fibrillation, aspirin is not effective enough. Guidelines no longer recommend it as a substitute for anticoagulation in seniors with AFib. Taking aspirin instead of a proper anticoagulant puts you at significantly higher stroke risk.
How often do I need blood tests if I’m on a DOAC?
Usually not at all. DOACs don’t require routine blood monitoring like warfarin does. But your doctor should check your kidney function every 6 to 12 months, especially if you’re over 75. If your creatinine clearance drops below 50 mL/min, your dose may need adjusting - particularly for dabigatran and edoxaban.
What if I need emergency surgery while on a DOAC?
There are reversal agents available. Idarucizumab reverses dabigatran within minutes. Andexanet alfa reverses apixaban, rivaroxaban, and edoxaban. These are used in emergencies like major bleeding or urgent surgery. Most hospitals now stock them. Your doctor should know your specific drug and have a plan in place.
If you’re caring for an elderly parent or loved one with AFib, the most important thing you can do is ask the doctor: “Are we doing everything we can to prevent a stroke - and how are we reducing fall risk?” Don’t accept fear as a reason to skip treatment. The evidence is solid. Anticoagulants save lives in seniors - even when they fall.






13 Comments
Simone Wood
November 21, 2025 AT 18:08Look, I get the fear. My mum fell last year, cracked her hip, and the doc said no more Eliquis because 'she's a fall risk.' But then she had a stroke six months later. No one talked about the real math: stroke kills faster than a bleed. We were scared of the wrong thing.
Anticoagulants aren't the enemy. Ignorance is.
And yes, I know apixaban is the gold standard for seniors. We switched her after reading this. She's still standing. Still alive. Still on meds.
Swati Jain
November 23, 2025 AT 09:07Let me just say this: if your doctor is still prescribing aspirin for AFib in 2025, fire them. Aspirin is like bringing a spoon to a hurricane. You’re not preventing a stroke-you’re just hoping for a miracle.
DOACs? Non-negotiable. Apixaban? The MVP. Kidney function? Check it. Home safety? Install grab bars. Exercise? Otago program, baby. Stop blaming the blood thinner. Start fixing the environment.
This isn’t medicine. This is common sense with a stethoscope.
Florian Moser
November 24, 2025 AT 18:15Excellent breakdown. The data is overwhelming: for every 100 seniors with AFib treated with DOACs, 24 strokes are prevented and only 3 major bleeds occur. That’s a 21:3 net benefit.
What’s missing from most clinical conversations is the psychological barrier. Doctors fear liability. Families fear guilt. But the real liability is inaction.
Apixaban’s 34% lower risk of intracranial hemorrhage versus warfarin is the clincher. And the fact that it’s dosed without monitoring makes it ideal for elderly patients with inconsistent lab access.
Bottom line: don’t stop the anticoagulant. Fix the fall risk. And if you’re not using CHA₂DS₂-VASc, you’re not practicing evidence-based medicine.
jim cerqua
November 26, 2025 AT 15:16OH MY GOD. I’ve been screaming this for years and everyone acts like I’m yelling at the moon.
My uncle was 89. Fell twice. Doctor said 'no blood thinners.' He had a stroke. Died in 72 hours. The hospital said 'we could’ve saved him.' But the doctor was scared of paperwork.
Now I’m watching my own mom get prescribed warfarin because 'it’s cheaper.' Do you know how many times she’s had to go for INR checks? 17 times in 6 months. She’s 82. She can’t even walk to the car without shaking.
DOACs are not a luxury. They’re a lifeline. And if your doctor won’t prescribe apixaban to an 85-year-old, they’re not a doctor-they’re a coward with a stethoscope.
Donald Frantz
November 28, 2025 AT 04:35Let’s get real. The 2023 JHM review calling this 'inappropriate practice' is a wake-up call. But why are we still having this conversation? The ACC/AHA/HRS guidelines have been clear since 2019. So why is only 48% of octogenarians on anticoagulants?
Because medicine is still stuck in the 1990s. Fear-based decision-making. Liability avoidance. 'We don’t want to be the one who caused the bleed.'
But here’s the truth: the bleed risk from DOACs is lower than the stroke risk from NOT taking them. Period.
And yes, apixaban is the best for seniors. 27% renal clearance? Perfect for age-related decline. Reversal agent available? Check. No INR? Check. Twice daily? So what? She’s already taking 12 other pills.
This isn’t debatable. It’s arithmetic.
Sammy Williams
November 30, 2025 AT 02:42My grandma’s on apixaban. She fell last week-slipped on the bathmat. Scared the crap out of us. But we didn’t stop the meds. We got her a non-slip mat, a shower chair, and signed her up for Otago. She’s doing squats with a water bottle now. Laughing about it.
It’s not about stopping the drug. It’s about stopping the panic.
Also-dabigatran is a nightmare for kidneys. Stick with apixaban if she’s over 75. Trust me. Been there.
Daisy L
December 1, 2025 AT 06:24Let me just say this-AMERICA’S MEDICAL SYSTEM IS BROKEN. We treat seniors like fragile china dolls instead of people who’ve lived 80 years and deserve to not die from a preventable stroke!
Aspirin?! Are you kidding me?! That’s like giving a toddler a butter knife to fight a bear!
And don’t even get me started on doctors who say 'she falls too much' like it’s a valid excuse! What are they gonna do-put her in a bubble? Lock her in a padded room?
Apixaban. Now. And fix the damn bathroom. That’s the plan. Not fear. Not inertia. Not BS.
Anne Nylander
December 2, 2025 AT 06:21So my dad had afib and they wanted to put him on warfarin. I said no. We switched to Eliquis. He fell last month-hit his head. We rushed him. They gave him the reversal agent. He’s fine. No stroke. No brain bleed.
Just wanted to say: don’t let fear win. Talk to your doc. Ask for apixaban. Get a grab bar. Do the exercises. It’s not hard. It’s just scary at first.
He’s still walking. Still cooking. Still yelling at the TV. That’s the goal, right?
Franck Emma
December 3, 2025 AT 00:11My mom died from a brain bleed on warfarin.
She was 81.
They told us 'it was just bad luck.'
It wasn’t.
It was negligence.
DOACs exist for a reason.
Don’t let your family die because someone was too lazy to update their playbook.
Paula Jane Butterfield
December 3, 2025 AT 02:54As a nurse who’s worked in geriatrics for 22 years, I’ve seen this over and over. Families panic. Doctors hesitate. And seniors pay the price.
Here’s the thing: falls don’t kill. Strokes do.
And the best way to prevent a stroke in AFib? Anticoagulation.
Apixaban is the safest for older adults. No need for blood tests. Lower brain bleed risk. Easy dosing.
And yes-fall risk? Fix the house. Add lights. Remove rugs. Do balance exercises. But don’t stop the medicine.
I’ve had patients on DOACs fall 5 times in a year and still walk out of the hospital. I’ve had others off meds get stroke #2 and never come home.
It’s not even close.
Noah Fitzsimmons
December 4, 2025 AT 02:32Oh, so now we’re pretending that anticoagulants are safe? Let me tell you about Mrs. Henderson. 88. On apixaban. Fell. Blew out her spleen. Died in the ER. The family sued. The hospital settled.
So what’s the real cost? A stroke? Maybe. But a $2M lawsuit? That’s the real fear.
Doctors aren’t ignoring guidelines-they’re avoiding lawsuits.
And don’t act like you’re some hero for pushing DOACs. You’re just gambling with someone’s life.
Aspirin isn’t perfect. But at least it doesn’t turn a slip into a funeral.
Eliza Oakes
December 5, 2025 AT 15:28Wait-you’re telling me we should give blood thinners to people who can’t even stand up without help? That’s not medicine. That’s reckless.
What about the 12% of seniors who have silent bleeds? The ones who don’t even know they’re bleeding internally until they collapse?
And you want to give them a drug that has no routine monitoring? Are you insane?
Maybe we should just stop pretending elderly people can handle modern medicine. Maybe we should just… let them go peacefully.
Instead of playing god with their anticoagulants.
Clifford Temple
December 6, 2025 AT 12:21Let me get this straight: we’re supposed to trust a pill over common sense? A 90-year-old with weak legs, bad vision, and a history of falls is going to be safer with a blood thinner than without?
That’s not science. That’s ideology.
And don’t give me that 'apixaban is safer' nonsense. It’s still a blood thinner. It still bleeds. It still kills.
Maybe we should stop treating seniors like lab rats and start treating them like human beings who deserve dignity in their final years-not a chemical gamble.
Aspirin isn’t perfect. But it’s honest. And it doesn’t turn a stumble into a death sentence.